Exhibits
Specify which potential condition the client is most likely experiencing, two actions the nurse should take to address that condition, and two parameters the nurse should monitor to assess the client’s response.
The Correct Answer is []
- The client is most likely experiencing compartment syndrome, which is a condition where increased pressure within a closed space compromises blood flow and tissue perfusion. Compartment syndrome can occur after a fracture, especially if a cast or splint is applied too tightly. Some of the signs and symptoms of compartment syndrome are severe pain, paresthesia, pallor, and pulselessness.
- Two actions the nurse should take to address compartment syndrome are:
- Elevate the extremity above the level of the heart to reduce swelling and improve venous return.
- Remove the cast or loosen the dressing to relieve the pressure and restore blood flow. This may require notifying the physician or obtaining an order for bivalving or cutting the cast.
- Two parameters the nurse should monitor to assess the client’s condition are:
- Capillary refill of the affected fingers, which should be less than 3 seconds. A prolonged capillary refill indicates poor perfusion and tissue ischemia.
- Blood pressure of the client, which should be maintained within normal limits. Hypotension can worsen the perfusion deficit and lead to tissue necrosis.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A reason: This is incorrect because monitoring pulse oximetry every 2 hours is not a sufficient or timely intervention for the nurse to implement. Pulse oximetry is a noninvasive method of measuring the oxygen saturation of hemoglobin in the blood. Normal oxygen saturation is 95% to 100%, while hypoxemia is less than 90%. However, pulse oximetry may not reflect the severity of respiratory distress or the effectiveness of nebulizer treatment in a client with asthma. Moreover, monitoring pulse oximetry every 2 hours is too infrequent for a client who is in acute respiratory distress and needs more frequent assessment and intervention.
Choice B reason: This is incorrect because teaching proper use of a rescue inhaler is not a priority or relevant intervention for the nurse to implement. A rescue inhaler is a type of short-acting bronchodilator that can be used to relieve acute asthma symptoms by relaxing the smooth muscles of the airways and improving airflow. However, teaching proper use of a rescue inhaler is not an urgent action for a client who is already receiving nebulizer treatment, which delivers a higher dose of medication directly to the lungs. Moreover, teaching proper use of a rescue inhaler is not appropriate for a client who is in respiratory distress and may not be able to focus or retain information.
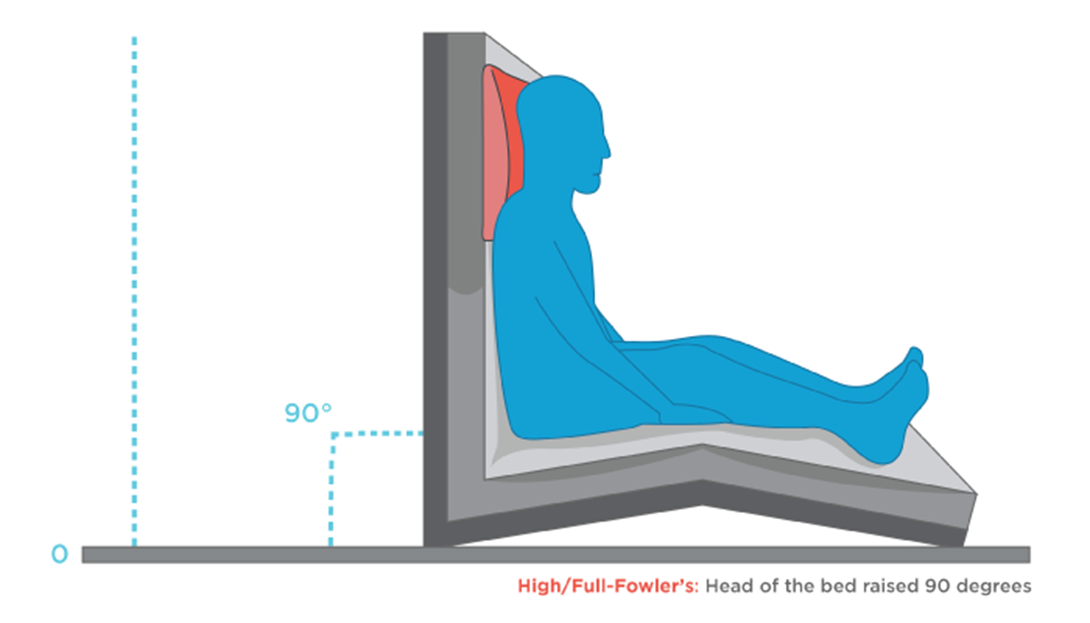
Choice C reason: This is correct because elevating the head of bed to 90 degrees is the most important intervention for the nurse to implement. Elevating the head of bed to 90 degrees can help improve breathing and oxygenation by reducing pressure on the diaphragm and chest wall, increasing lung expansion and ventilation, and facilitating expectoration of mucus. This can enhance the effects of nebulizer treatment and reduce respiratory distress in a client with asthma.
Choice D reason: This is incorrect because determining exposure to asthmatic triggers is not an immediate or helpful intervention for the nurse to implement. Asthmatic triggers are substances or factors that can cause or worsen asthma symptoms by inducing inflammation or constriction of the airways. Examples of asthmatic triggers include allergens, irritants, infections, exercise, stress, or weather changes. However, determining exposure to asthmatic triggers is not a priority action for a client who is in respiratory distress and needs more urgent interventions to improve breathing and oxygenation. Moreover, determining exposure to asthmatic triggers may not change the management or outcome of an acute asthma attack that has already occurred.
Correct Answer is A
Explanation
Choice A reason: This is correct because performing a bedside pregnancy test is the intervention that should be implemented immediately by the nurse. This is to confirm or rule out pregnancy and inform the surgical team of any possible risks or complications that may affect the client or the fetus.
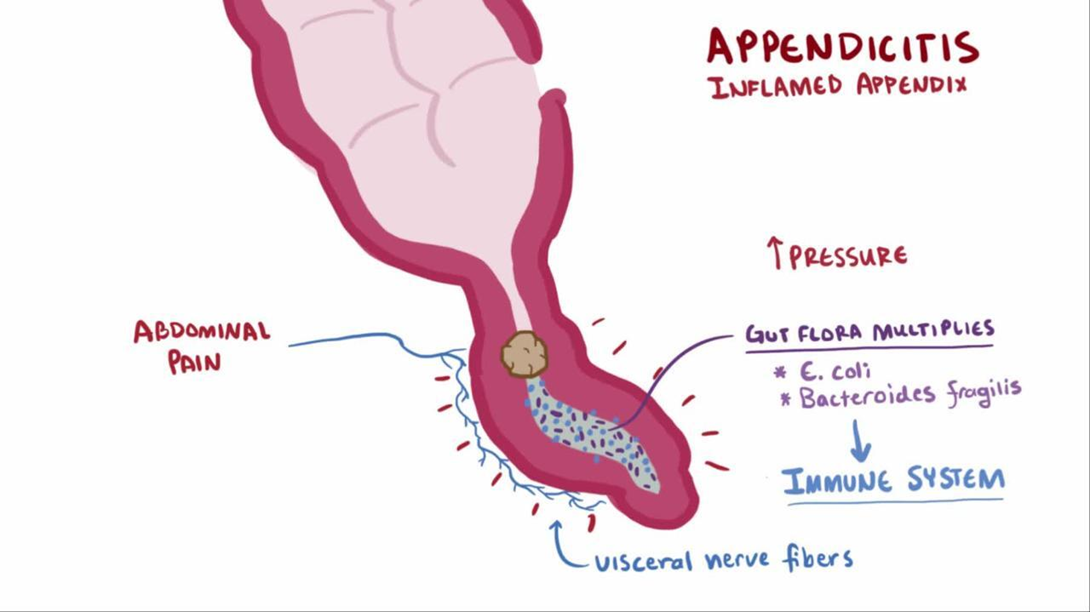
Choice B reason: This is incorrect because continuing with surgery as scheduled is not an appropriate intervention without verifying the pregnancy status of the client. Surgery may pose serious threats to both maternal and fetal health, such as bleeding, infection, anesthesia complications, or miscarriage.
Choice C reason: This is incorrect because calculating gestation from last menstrual cycle is not an accurate or reliable method of determining pregnancy. The menstrual cycle can vary widely among women and may be affected by various factors such as stress, illness, or medication.
Choice D reason: This is incorrect because notifying the surgical team to cancel the surgery is not a necessary intervention unless pregnancy is confirmed. Appendicitis is a medical emergency that requires prompt surgical treatment to prevent rupture, peritonitis, or sepsis.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
