Days after surgical fixation of a fractured femur, a client suddenly reports chest pain and difficulty in breathing. The nurse suspects that the client had a pulmonary embolus. Which action should the nurse take first?
Notify the healthcare provider.
Prepare a continuous heparin infusion per protocol.
Provide supplemental oxygen.
Bring the emergency crash cart to the bedside.
The Correct Answer is C
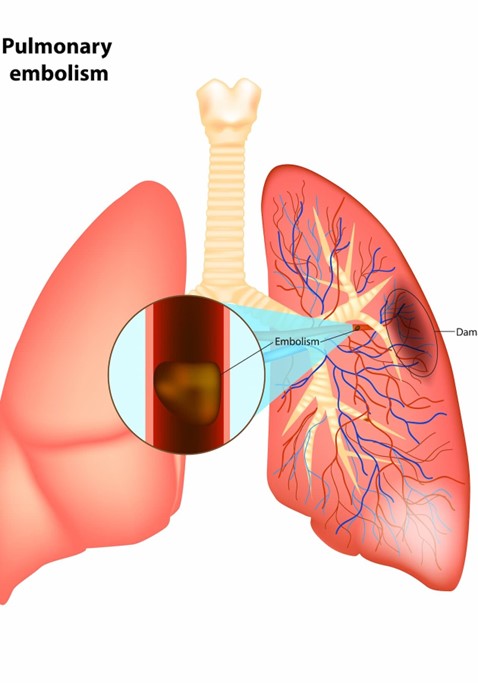
Choice C is correct because providing supplemental oxygen is the first action that the nurse should take for a client who has a suspected pulmonary embolus. A pulmonary embolus is a life-threatening condition that occurs when a blood clot travels to the lungs and blocks the blood flow, causing hypoxia and respiratory distress. The nurse should administer oxygen to improve the client's oxygenation and prevent further complications.
Choice A is incorrect because notifying the healthcare provider is not the first action that the nurse should take for a client who has a suspected pulmonary embolus. The nurse should notify the healthcare provider after providing supplemental oxygen and assessing the client's vital signs and symptoms.
Choice B is incorrect because preparing a continuous heparin infusion per protocol is not the first action that the nurse should take for a client who has a suspected pulmonary embolus. Heparin is an anticoagulant that can prevent further clot formation and reduce the risk of recurrence, but it does not dissolve existing clots or improve oxygenation. The nurse should prepare a heparin infusion after obtaining a prescription from the healthcare provider and confirming the diagnosis with diagnostic tests.
Choice D is incorrect because bringing the emergency crash cart to the bedside is not the first action that the nurse should take for a client who has a suspected pulmonary embolus. The emergency crash cart contains equipment and medications that can be used in case of cardiac arrest or other emergencies, but it does not address the immediate need of oxygenation. The nurse should bring the emergency crash cart to the bedside after providing supplemental oxygen and assessing the client's condition.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice B reason: Erythrocytes, hemoglobin, and hematocrit are laboratory results that are not as critical as serum potassium, calcium, and phosphorus in a client who has end-stage renal disease (ESRD.. Erythrocytes are red blood cells that carry oxygen from the lungs to the tissues. Hemoglobin is a protein in erythrocytes that binds oxygen. Hematocrit is the percentage of blood volume that is occupied by erythrocytes. ESRD can cause anemia (low erythrocyte, hemoglobin, and hematocrit levels) due to reduced production of erythropoietin, a hormone that stimulates erythrocyte formation, by the kidneys. Anemia can cause fatigue, pallor, or shortness of breath.
Choice C reason: Leukocytes, neutrophils, and thyroxine are laboratory results that are not as relevant as serum potassium, calcium, and phosphorus in a client who has end-stage renal disease (ESRD.. Leukocytes are white blood cells that fight infection and inflammation. Neutrophils are a type of leukocyte that respond to bacterial infection. Thyroxine is a hormone that regulates metabolism and growth. ESRD can cause leukopenia (low leukocyte levels) and neutropenia (low neutrophil levels) due to impaired immune function and increased susceptibility to infection. ESRD can also cause hypothyroidism (low thyroxine levels) due to reduced clearance of thyroid hormones by the kidneys. Hypothyroidism can cause weight gain, cold intolerance, or depression.
Choice D reason: Blood pressure, heart rate, and temperature are not laboratory results, but vital signs that should be monitored in a client who has end-stage renal disease (ESRD.. Blood pressure is the force of blood against the walls of the arteries. Heart rate is the number of times the heart beats per minute. Temperature is the measure of body heat. ESRD can cause hypertension (high blood pressurE. due to fluid overload and activation of the renin-angiotensin-aldosterone system, a hormonal pathway that regulates blood pressure and fluid balance. Hypertension can cause headache, chest pain, or stroke. ESRD can also cause tachycardia (high heart ratE. due to anemia, fluid overload, or electrolyte imbalance. Tachycardia can cause palpitations, dizziness, or heart failure. ESRD can also cause fever (high temperaturE. due to infection or inflammation. Fever can cause chills, sweating, or delirium.
Correct Answer is A
Explanation
Choice A is correct because the nurse's priority is to provide comfort and dignity to the dying patient. Pain management is an essential aspect of end-of-life care.
Choice B is incorrect because updating the nurse manager is not a priority action. The nurse manager can be informed later, after the patient's needs are met.
Choice C is incorrect because conveying the patient's status to the chaplain is not a priority action. The chaplain can be contacted later, after the patient's needs are met. The chaplain may also need the consent of the patient or the family before providing spiritual support.
Choice D is incorrect because documenting the impending signs of death is not a priority action. Documentation can be done later, after the patient's needs are met. Documentation is important, but not as important as providing comfort and dignity to the dying patient.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
