An older client with a history of heart failure and admitted to the medical unit after falling at home and has become increasingly confused. The client's spouse is designated as the client's power of attorney.
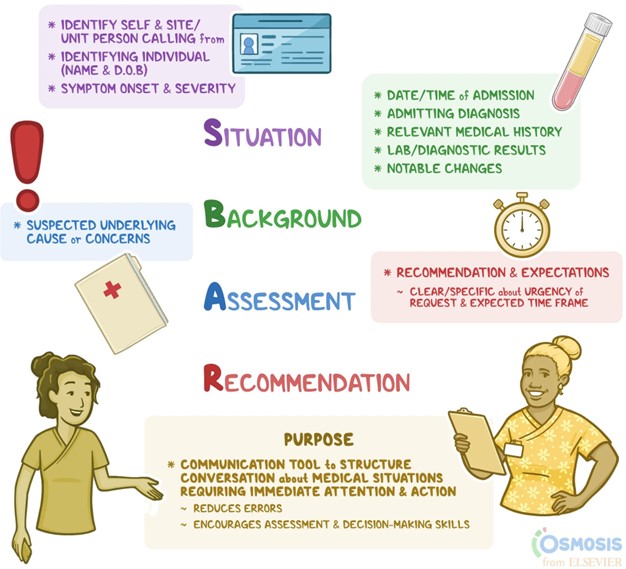
When reporting to the healthcare provider using SBAR (Situation, Background, Assessment, Recommendation) communication, which information should the nurse provide first?
Currently prescribed medications.
Fall at home as reason for admission.
Client's healthcare power of attorney.
Increasing confusion of the client.
The Correct Answer is D
Situation: Increasing confusion of the client.
The nurse should start by providing the current situation, which is the client's increasing confusion. This is crucial information as it indicates a change in the client's condition and may require immediate attention.
Background: Fall at home as reason for admission.
Next, the nurse should provide the background information, which includes the reason for admission, in this case, the fall at home. This helps the healthcare provider understand the context and potential contributing factors to the client's current condition. Assessment: Currently prescribed medications.
After providing the background, the nurse should discuss the assessment findings. In this case, it would be appropriate to mention the client's currently prescribed medications. This information can help the healthcare provider assess for any medication-related issues or interactions that could be contributing to the client's confusion.
Recommendation: Client's healthcare power of attorney.
Lastly, the nurse should provide the recommendation, which in this case is the client's healthcare power of attorney. This information is important as it identifies the designated decision-maker for the client's healthcare decisions and can assist the healthcare provider in involving the appropriate person in the care planning process.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Itraconazole is an antifungal medication used to treat a variety of fungal infections. Antacids, which are used to treat heartburn and acid reflux, can decrease the absorption of itraconazole in the body. Therefore, it is important to instruct the client to avoid taking itraconazole with antacids. If the client needs to take an antacid, it should be taken at least 2 hours before or after taking itraconazole.
Reporting any difficulty with breathing is important as it can be a sign of an allergic reaction to the medication. Monitoring for changes in stool color is important as it can be an indication of liver dysfunction, which is a potential side effect of itraconazole.
Avoiding the consumption of grapefruit juice is important as it can increase the level of itraconazole in the body, which can increase the risk of side effects.
In summary, the client should be instructed to avoid taking itraconazole with antacids and to take any antacid at least 2 hours before or after taking itraconazole. The client should also be instructed to report any difficulty with breathing and to monitor for changes in stool color. Additionally, the client should avoid consuming grapefruit juice while taking itraconazole.
Correct Answer is ["1000"]
Explanation
rate (mL/h) = volume (mL) / time (h).
In this case, the volume is 500 mL and the time is 0.5 h (30 minutes).
Plugging these values into the formula, we get: rate (mL/h) = 500 mL / 0.5 h = 1000 mL/h. Therefore, the nurse should set the infusion pump to 1000 mL/hour.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
