A woman comes to the prenatal clinic suspecting that she is pregnant, and assessment reveals probable signs of pregnancy. Which findings would the nurse most likely assess? Select all that apply.
Ultrasound visualization of the fetus
Softening of the cervix
Positive pregnancy test
Absence of menstruation
Ballottement
Auscultation of a fetal heart beat
Correct Answer : B,C,D,E
Choice A Reason: This is incorrect because ultrasound visualization of the fetus is a positive sign of pregnancy, not a probable sign. A positive sign of pregnancy is a direct and definitive evidence of the presence of a fetus, such as fetal movement felt by the examiner or fetal heart sounds heard by a Doppler device.
Choice B Reason: This is correct because softening of the cervix, also known as Goodell's sign, is a probable sign of pregnancy. A probable sign of pregnancy is a strong indication of pregnancy based on physical changes in the reproductive organs, such as enlargement of the uterus or changes in the shape and consistency of the cervix.
Choice C Reason: This is correct because a positive pregnancy test, which detects human chorionic gonadotropin (hCG) in urine or blood, is a probable sign of pregnancy. However, it is not a conclusive sign, as hCG can also be produced by other conditions such as ectopic pregnancy, molar pregnancy, or trophoblastic tumors.
Choice D Reason: This is correct because absence of menstruation, also known as amenorrhea, is a probable sign of pregnancy. It occurs when ovulation and menstruation cease due to hormonal changes during pregnancy. However, it is not a definitive sign, as amenorrhea can also be caused by other factors such as stress, illness, or hormonal imbalances.
Choice E Reason: This is correct because ballottement, which is a rebounding of the fetus against the examiner's fingers during a pelvic examination, is a probable sign of pregnancy. It can be felt around 16 to 20 weeks of gestation.
Choice F Reason: This is incorrect because auscultation of a fetal heart beat, which can be heard by a fetoscope around 18 to 20 weeks of gestation or by a Doppler device around 10 to 12 weeks of gestation, is a positive sign of pregnancy, not a probable sign.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A Reason: Linea nigra is a dark vertical line that appears on the abdomen of some pregnant women. It is caused by increased melanin production and usually fades after delivery.
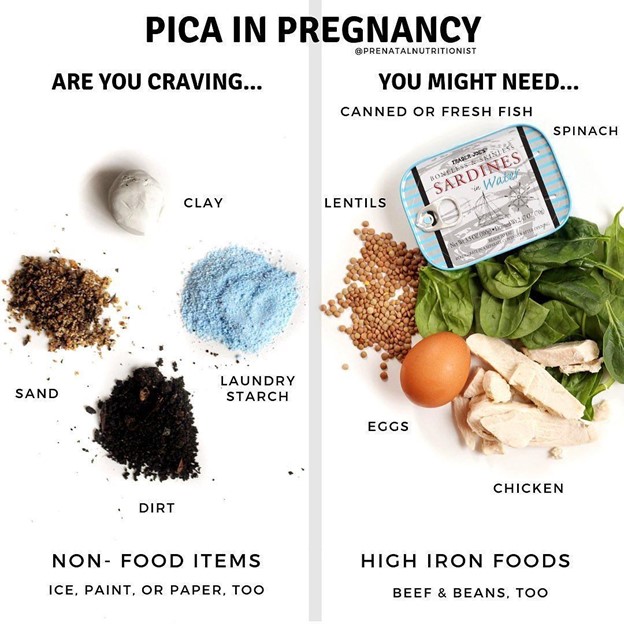
Choice B Reason: Pica is a condition in which a person has an abnormal desire to eat substances that are not food, such as ice, clay, dirt, or chalk. It is more common in pregnant women and may indicate a deficiency in iron or other nutrients.
Choice C Reason: Ballottement is a technique of palpating a floating structure by bouncing it gently and feeling it rebound. In obstetrics, it can be used to detect the presence of the fetus by feeling its head move when the cervix is tapped.
Choice D Reason: Quickening is the first perception of fetal movements by the pregnant woman. It usually occurs between 16 and 20 weeks of gestation.
Correct Answer is B
Explanation
Choice A Reason: This is incorrect because wearing spandex-type full-length pants can constrict the blood flow and increase the swelling in the feet. The nurse should advise the woman to wear loose-fitting clothes and comfortable shoes that do not squeeze or rub her feet.
Choice B Reason: This is correct because elevating the legs when sitting can improve venous return and reduce the swelling in the feet. The nurse should encourage the woman to elevate her legs above her heart level whenever possible and avoid crossing her legs or standing for long periods.
Choice C Reason: This is incorrect because limiting the intake of fluids can cause dehydration and worsen the swelling in the feet. The nurse should recommend the woman drink plenty of water and other healthy fluids to maintain hydration and flush out excess sodium and waste products from her body.
Choice D Reason: This is incorrect because eliminating salt from the diet can cause electrolyte imbalance and affect the fluid balance in the body. The nurse should advise the woman to consume salt in moderation and avoid processed foods that are high in sodium.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
