A patient is admitted to the hospital with symptoms consistent with a right hemisphere stroke. Which neurovascular assessment requires immediate intervention by the nurse?
Pupillary changes to ipsilateral dilation.
Left-sided facial drooping and dysphagia.
Orientation to person and place only.
Unequal bilateral hand grip strengths.
The Correct Answer is A
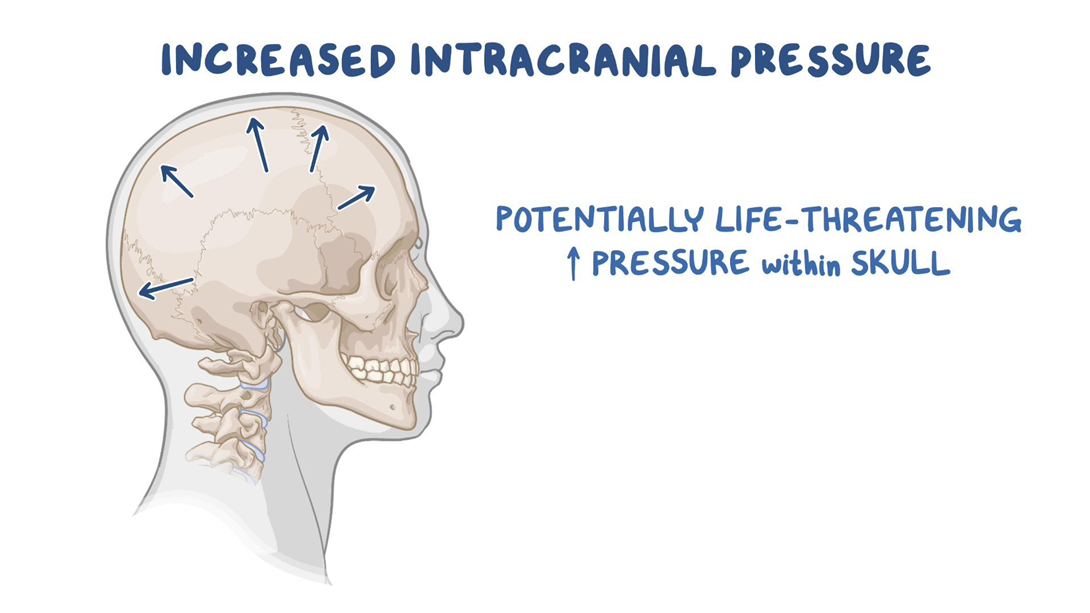
Choice A reason: Pupillary changes to ipsilateral dilation indicate increased intracranial pressure, which is a life-threatening complication of stroke. The nurse should notify the physician and prepare for emergency measures.
Choice B reason: Left-sided facial drooping and dysphagia are common signs of right hemisphere stroke, but they do not require immediate intervention by the nurse. The nurse should monitor the patient's swallowing ability and provide oral care.
Choice C reason: Orientation to person and place only is a sign of impaired cognition, which is also common in right hemisphere stroke. The nurse should assess the patient's memory, judgment, and attention span.
Choice D reason: Unequal bilateral hand grip strengths are a sign of hemiparesis, which is a weakness on one side of the body. The nurse should assist the patient with mobility and prevent contractures.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A reason: A referral for social services at home is not necessary for a client with Addison's disease who has stable vital signs, adequate hydration, and good self-care knowledge.
Choice B reason: Limiting daily fluid intake to 500 mL is not appropriate for a client with Addison's disease, who is at risk of dehydration and hypotension. The client should drink fluids according to thirst and urine output.
Choice C reason: Preparing the client for discharge home is the best action for the nurse to implement, as the client has no signs of complications or deterioration from Addison's disease. The client should be able to manage the condition at home with regular follow-up and medication adherence.
Choice D reason: Strict intake and output monitoring is not required for a client with Addison's disease who has normal blood pressure, moist mucous membranes, and strong peripheral pulses. These indicate adequate fluid balance and renal function.
Correct Answer is B
Explanation
Choice A reason: Obtaining a soft diet for the client is not the best initial nursing action for a client with chemotherapy-induced mucositis who is describing soreness of the tongue and oral issues. A soft diet can help reduce the irritation and discomfort of the oral mucosa, but it does not address the underlying cause of the inflammation and infection. The nurse should first assess the client's oral hygiene and provide appropriate interventions to prevent further complications.
Choice B reason: Encouraging frequent mouth care is the best initial nursing action for a client with chemotherapy-induced mucositis who is describing soreness of the tongue and oral issues. Frequent mouth care can help prevent or reduce the severity of mucositis by removing plaque, bacteria, and debris from the oral cavity, and by moisturizing and soothing the oral tissues. The nurse should instruct the client to use a soft toothbrush, a mild toothpaste, and a saline or bicarbonate rinse at least four times a day, and to avoid alcohol, tobacco, spicy, acidic, or hot foods and beverages.
Choice C reason: Cleansing the tongue and mouth with swabs is not the best initial nursing action for a client with chemotherapy-induced mucositis who is describing soreness of the tongue and oral issues. Swabs can be abrasive and damaging to the oral mucosa, especially if they are dry or contain alcohol or hydrogen peroxide. Swabs can also increase the risk of bleeding, infection, and ulceration of the oral tissues. The nurse should use a soft toothbrush or a gentle sponge to clean the tongue and mouth.
Choice D reason: Administering a topical analgesic per protocol is not the best initial nursing action for a client with chemotherapy-induced mucositis who is describing soreness of the tongue and oral issues. A topical analgesic can provide temporary relief of pain and discomfort, but it does not address the underlying cause of the inflammation and infection. The nurse should first assess the client's oral hygiene and provide appropriate interventions to prevent further complications. The nurse should also monitor the client's response to the analgesic and report any adverse effects or inadequate pain control.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
