A nurse is reviewing the medical record of a client who has a prescription for misoprostol for induction of labor.
Which of the following findings is a contraindication for administration of this medication?
Preeclampsia.
Transverse fetal lie.
Intrauterine growth restriction.
Postterm pregnancy.
The Correct Answer is B
Choice A rationale:
Preeclampsia is not a contraindication for the administration of misoprostol for induction of labor. Misoprostol is a prostaglandin E1 analog used for cervical ripening and induction of labor. It is not contraindicated in patients with preeclampsia. However, its use should be carefully monitored in patients with hypertensive disorders of pregnancy due to the potential impact on blood pressure.
Choice B rationale:
Transverse fetal lie is a contraindication for the administration of misoprostol for induction of labor. Misoprostol should not be used when the baby is in a transverse position because it can lead to complications during delivery. Induction methods should be chosen carefully based on the fetal presentation to ensure a safe delivery process.
Choice C rationale:
Intrauterine growth restriction (IUGR) is not a contraindication for the administration of misoprostol for induction of labor. IUGR refers to a condition where a fetus does not grow at the expected rate inside the uterus. While the cause of IUGR needs to be addressed, misoprostol itself is not contraindicated in these cases. However, the healthcare provider should assess the overall fetal well-being before deciding on the induction method.
Choice D rationale:
Postterm pregnancy is not a contraindication for the administration of misoprostol for induction of labor. In postterm pregnancies, where the pregnancy has extended beyond 42 weeks, healthcare providers may consider inducing labor to prevent complications associated with prolonged gestation. Misoprostol is one of the options for induction in postterm pregnancies, although the choice of induction method may vary based on various factors.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
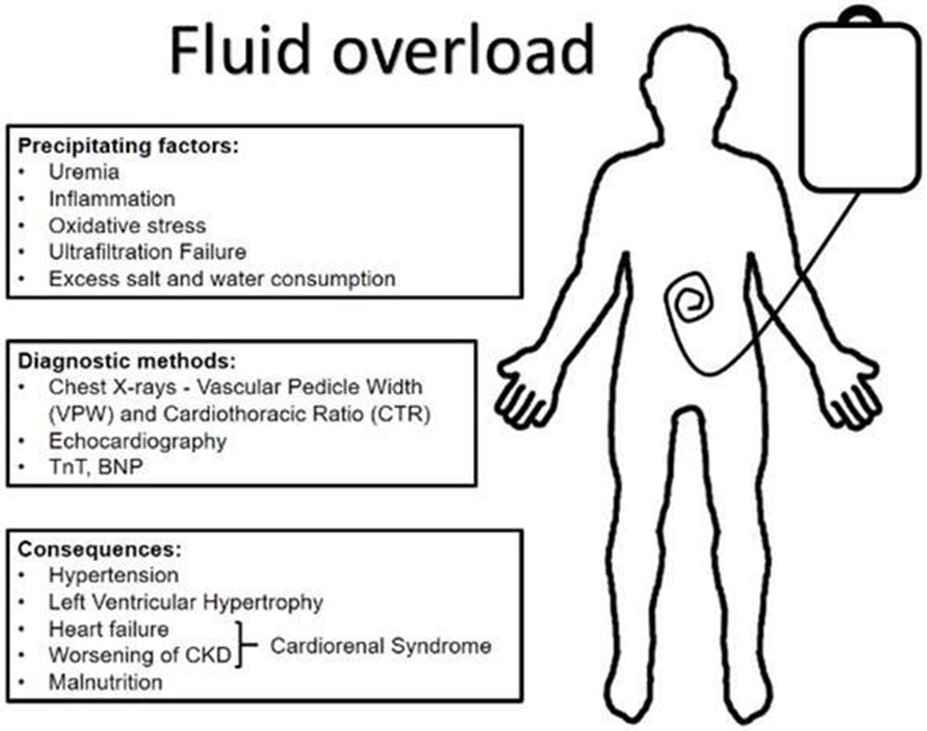
- A. Oliguria. This is incorrect because oliguria, or decreased urine output, is a sign of fluid volume deficit, not fluid volume overload.
- B. Bradycardia. This is incorrect because bradycardia, or slow heart rate, is not a typical sign of fluid volume overload, unless the client has a cardiac condition that affects the heart's response to fluid overload.
- C. Dyspnea. This is correct because dyspnea, or difficulty breathing, is a common sign of fluid volume overload, as excess fluid accumulates in the lungs and impairs gas exchange.
- D. Poor skin turgor. This is incorrect because poor skin turgor, or decreased elasticity of the skin, is a sign of dehydration, not fluid volume overload.
Correct Answer is A
Explanation
- A is correct because delegating non-nursing tasks to ancillary staff allows nurses to focus on more complex and skilled tasks that require their expertise and judgment, thus improving efficiency and quality of care.
- B is incorrect because stocking client rooms with extra supplies increases waste and costs, as well as clutter and infection risk.
- C is incorrect because assigning dedicated equipment to each client's room reduces availability and accessibility of equipment for other clients, as well as increases maintenance and cleaning costs.
- D is incorrect because changing continuous IV infusion tubing every 24 hr is not cost-effective, as it does not reduce the risk of infection significantly compared to changing it every 72 hr, according to current evidence-based practice guidelines.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
