A nurse is providing teaching to a client who has type 1 diabetes mellitus. Which of the following statements by the client indicates an understanding of the teaching?
"I will have ketones in my urine if my blood glucose is maintained at 190 milligrams per deciliter."
"I will keep my blood glucose levels between 200 and 212 milligrams per deciliter."
"I will keep my HbA1c at five percent."
"Albumin in my urine is an indication of normal kidney function."
The Correct Answer is A
In type 1 diabetes mellitus, when blood glucose levels are consistently high, the body may start breaking down fat for energy, leading to the production of ketones. Ketones can be detected in urine as a result. A blood glucose level of 190 milligrams per deciliter is elevated and can potentially trigger the production of ketones. Monitoring urine for ketones can be an important indicator of diabetes management and helps identify potential complications.
The other statements by the client indicate a lack of understanding or potential misconceptions:
● "I will keep my blood glucose levels between 200 and 212 milligrams per deciliter": This statement suggests a target range that is higher than the recommended target blood glucose levels for individuals with diabetes. Generally, the target range for blood glucose levels in individuals with diabetes is lower, typically between 80-130 mg/dL before meals and below 180 mg/dL after meals.
● "Albumin in my urine is an indication of normal kidney function": This statement is incorrect. The presence of albumin in the urine, called albuminuria, is an indication of kidney damage or dysfunction. It is a common sign of kidney disease, including diabetic nephropathy, which is a complication of diabetes affecting the kidneys.
● "I will keep my HbA1c at five percent": While maintaining a lower HbA1c level is generally desirable for individuals with diabetes, a target of five percent is too low. HbA1c is a measure of average blood glucose levels over the past two to three months. The American Diabetes Association (ADA) recommends an HbA1c target of less than 7 percent for most adults with diabetes, although individualized targets may vary based on factors such as age and other health conditions.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
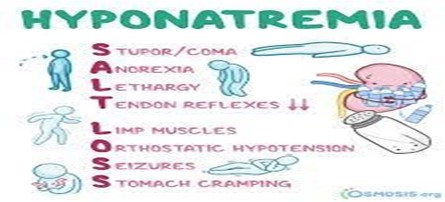
Muscle weakness is a finding that indicates the client is experiencing water intoxication. Muscle weakness is a symptom of water intoxication because the excessive intake of water dilutes the sodium levels in the blood, causing hyponatremia. Sodium is an electrolyte that helps maintain the balance of fluids in and around cells and also regulates muscle contraction. When sodium levels are too low, the cells swell and the muscles lose their ability to function properly.
Weak pulses are not a specific finding for water intoxication, as they can be caused by other factors such as decreased blood volume or inadequate cardiac output.
Hypernatremia is the opposite of hyponatremia, meaning high sodium levels in the blood. This can occur due to dehydration, excessive salt intake, or certain medical conditions, but not water intoxication.
Exaggerated reflexes are not typically associated with water intoxication. They may be seen in conditions such as hyperreflexia or certain neurological disorders.
Correct Answer is C
Explanation
The nurse should plan to change the IV tubing for the TPN solution every 72 hours. This is necessary to maintain the sterility of the system and minimize the risk of infection. TPN solutions are prone to bacterial growth, and changing the tubing regularly helps prevent contamination.
Removing TPN from the refrigerator 5 minutes before infusing it is not necessary. TPN solutions are typically stored in the refrigerator to maintain their stability and prevent spoilage. It should be brought to room temperature over a longer period of time, usually 30-60 minutes, before administration.
Discarding the remaining TPN solution that is still infusing after 24 hours is unnecessary. TPN solutions can typically be infused for up to 24 hours without compromising their safety and efficacy. However, it is important to monitor the solution closely for any signs of contamination or degradation, and if any concerns arise, the nurse should consult with the healthcare provider.
Changing the dressing around the IV site weekly is not specific to TPN administration. Dressing changes for peripheral IV sites are typically performed according to facility protocols and the condition of the site, but they are not necessarily done on a weekly basis. The frequency of dressing changes depends on factors such as the type of dressing used, the patient's condition, and any signs of infection or dislodgement.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
