A nurse is providing care for a client who has the syndrome of inappropriate antidiuretic hormone (SIADH). Which of the following findings is consistent with a diagnosis of SIADH?
Increased serum sodium
Decreased serum osmolality
Decreased urinary sodium
Decreased urine osmolality
The Correct Answer is B
Choice A reason: Increased Serum Sodium
Increased serum sodium, or hypernatremia, is not consistent with SIADH. SIADH typically results in hyponatremia, which is a low level of sodium in the blood due to excessive water retention. The excess antidiuretic hormone (ADH) causes the kidneys to retain water, diluting the sodium in the bloodstream. Therefore, increased serum sodium is not a characteristic finding in SIADH.
Choice B reason: Decreased Serum Osmolality
Decreased serum osmolality is a hallmark of SIADH3. Serum osmolality measures the concentration of solutes in the blood. In SIADH, the excessive release of ADH leads to water retention, diluting the blood and lowering serum osmolality. This is a key diagnostic feature of SIADH and helps differentiate it from other conditions.
Choice C reason: Decreased Urinary Sodium
Decreased urinary sodium is not typically seen in SIADH. In fact, patients with SIADH usually have increased urinary sodium levels. This is because the kidneys excrete more sodium in an attempt to balance the excess water retained due to high ADH levels. Therefore, decreased urinary sodium is not consistent with SIADH.
Choice D reason: Decreased Urine Osmolality
Decreased urine osmolality is also not consistent with SIADH. In SIADH, urine osmolality is typically increased because the kidneys concentrate the urine due to the action of ADH. The high levels of ADH cause the kidneys to reabsorb water, resulting in more concentrated urine. Thus, decreased urine osmolality is not a characteristic finding in SIADH.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason:
Decreasing activity is not recommended for managing peripheral venous disease. Regular physical activity, such as walking, helps improve blood circulation and can reduce symptoms. Inactivity can lead to worsening of the condition and increase the risk of complications.
Choice B Reason:
Massaging the legs frequently is not typically recommended for preventing fluid buildup in peripheral venous disease. Instead, compression therapy, such as wearing compression stockings, is more effective in managing symptoms and preventing fluid accumulation.
Choice C Reason:
Keeping the legs in a dependent position (hanging down) can worsen symptoms of peripheral venous disease. Elevating the legs above heart level helps reduce swelling and improve blood flow, which is beneficial for managing the condition.
Choice D Reason:
Inspecting the legs daily for changes in color, size, and temperature is crucial for managing peripheral venous disease. This practice helps in early detection of complications such as infections, ulcers, or worsening of the condition, allowing for timely medical intervention.
Correct Answer is A
Explanation
Choice A Reason:
Swollen and enlarged veins, also known as varicose veins, are a common manifestation of peripheral venous disease (PVD). This condition occurs when the valves in the veins become weak or damaged, leading to blood pooling and increased pressure within the veins. This results in the veins becoming enlarged, twisted, and visible under the skin1. Varicose veins can cause discomfort, pain, and a heavy feeling in the legs. They are often exacerbated by prolonged standing or sitting and can be a cosmetic concern as well.
Choice B Reason:
Loss of pigmentation over the shin area is not typically associated with peripheral venous disease. This symptom is more commonly seen in conditions such as chronic venous insufficiency (CVI), where prolonged venous hypertension leads to skin changes, including hyperpigmentation and lipodermatosclerosis. However, it is not a primary manifestation of PVD itself.
Choice C Reason:
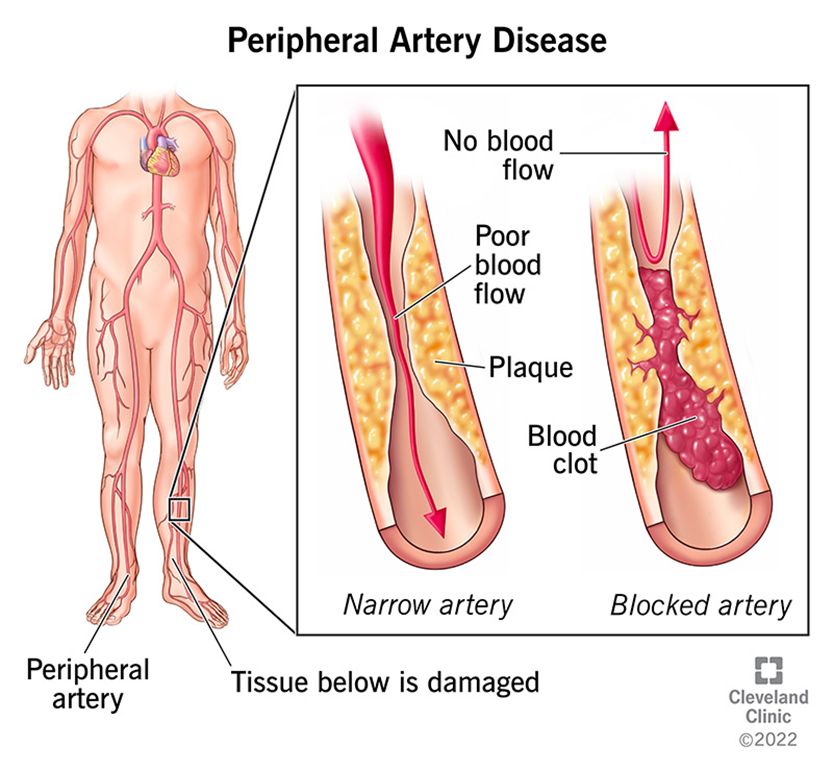
A shiny appearance to the lower extremities is more commonly associated with peripheral arterial disease (PAD) rather than peripheral venous disease. In PAD, reduced blood flow to the extremities can cause the skin to become thin, shiny, and hairless. This is due to the lack of oxygen and nutrients reaching the skin and underlying tissues. In contrast, PVD primarily affects the veins and does not typically cause these skin changes.
Choice D Reason:
Diminished hair growth on the lower extremities is another symptom more commonly associated with peripheral arterial disease (PAD). In PAD, the reduced blood flow to the extremities can lead to hair loss, as the hair follicles do not receive adequate oxygen and nutrients. Peripheral venous disease, on the other hand, does not usually cause hair loss. Instead, it is characterized by symptoms related to venous insufficiency, such as varicose veins, swelling, and skin changes.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
