A nurse is providing discharge teaching for a client who was admitted with diabetes insipidus. Which of the following teaching topics should be prioritized?
Frequency of urination
Change in appetite
Benefit of medical alert bracelet
Weight gain or loss
The Correct Answer is C
Choice A Reason:
While monitoring the frequency of urination is important for managing diabetes insipidus, it is not the most critical aspect of discharge teaching. Diabetes insipidus causes excessive urination, and patients should be aware of this symptom. However, understanding the importance of wearing a medical alert bracelet is more crucial for ensuring immediate and appropriate care in emergencies.
Choice B Reason:
Changes in appetite are not a primary concern for patients with diabetes insipidus. The condition primarily affects fluid balance and urine output rather than appetite. Therefore, this topic is less relevant compared to the need for a medical alert bracelet.
Choice C Reason:
The benefit of a medical alert bracelet is paramount for patients with diabetes insipidus. In case of an emergency, the bracelet can inform healthcare providers about the patient’s condition, ensuring they receive appropriate and timely treatment. This can be life-saving, especially if the patient is unable to communicate their medical history.
Choice D Reason:
Weight gain or loss can be a secondary concern for patients with diabetes insipidus, as the condition primarily affects fluid balance. While it is important to monitor weight to assess fluid status, it is not as critical as ensuring the patient understands the importance of wearing a medical alert bracelet.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
The correct answer is a. Insulin is stable at room temperature for one month.
Choice A Reason:
Insulin is stable at room temperature (between 59°F and 86°F) for up to one month. This is important for patients to know, especially if they do not have immediate access to refrigeration. However, it is crucial to avoid exposing insulin to extreme temperatures, such as direct sunlight or freezing conditions, as these can degrade the medication’s effectiveness.
Choice B Reason:
While some types of insulin can be mixed in the same syringe, this practice is not universally applicable to all insulin types. For example, rapid-acting and intermediate-acting insulins can sometimes be mixed, but long-acting insulins should not be mixed with other insulins. Therefore, this statement is not entirely accurate and should be clarified based on the specific types of insulin being used.
Choice C Reason:
Storing insulin in the freezer is not recommended as freezing can damage the insulin, rendering it ineffective. Insulin should be stored in a refrigerator at temperatures between 36°F and 46°F. If insulin is accidentally frozen, it should not be used.
Choice D Reason:
While it is advisable for clients with type 1 diabetes to have backup medication and supplies, storing them in a car is not recommended due to the potential for extreme temperature fluctuations. Insulin and other diabetes supplies should be kept in a stable, controlled environment to ensure their efficacy.
Correct Answer is A
Explanation
Choice A: Dietary and Fluid Restrictions
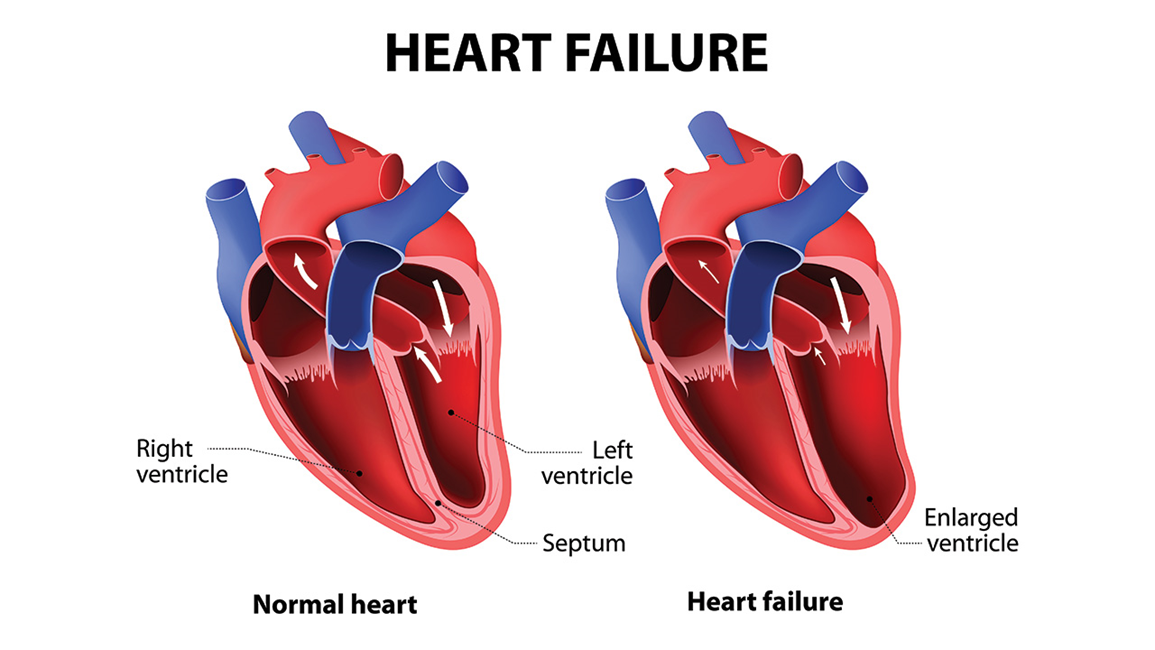
Dietary and fluid restrictions are crucial for patients with heart failure. These restrictions help manage symptoms and prevent complications. Limiting sodium intake can reduce fluid retention, which decreases the workload on the heart. Fluid restrictions help prevent fluid overload, which can lead to worsening heart failure symptoms. Patients are often advised to monitor their weight daily to detect fluid retention early. This choice is essential for managing heart failure effectively.
Choice B: Encouraging Increased Mobility
While physical activity is generally beneficial for overall health, it must be approached cautiously in patients with heart failure. Encouraging increased mobility without proper medical guidance can lead to overexertion and exacerbate heart failure symptoms. Exercise programs for heart failure patients should be tailored and supervised by healthcare professionals to ensure safety and effectiveness. Therefore, this choice is not as immediately critical as dietary and fluid restrictions.
Choice C: Cessation of Hormonal Supplements
Hormonal supplements can have various effects on the cardiovascular system, but their cessation is not a standard recommendation for all heart failure patients. The impact of hormonal supplements depends on the specific type and the patient’s overall health condition. This choice is less relevant compared to dietary and fluid restrictions, which have a direct and significant impact on heart failure management.
Choice D: Cessation of Intravenous (IV) Drug Use
Cessation of intravenous drug use is important for overall health and preventing infections, but it is not specific to heart failure management. While IV drug use can lead to complications that may affect the heart, it is not a primary lifestyle modification recommended for heart failure patients. The focus should be on managing fluid balance and dietary intake
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
