A nurse is collecting data on a client who has obstructive sleep apnea. Which of the following findings should the nurse expect?
Constipation
Nausea
Headache
Hypotension
The Correct Answer is C
A. Constipation
Constipation is not typically associated with obstructive sleep apnea. However, sleep disturbances and certain medications used to manage OSA may indirectly contribute to constipation in some cases.
B. Nausea
Nausea is not a common symptom of obstructive sleep apnea. While sleep disturbances may affect gastrointestinal function in some individuals, nausea is not a typical manifestation of OSA.
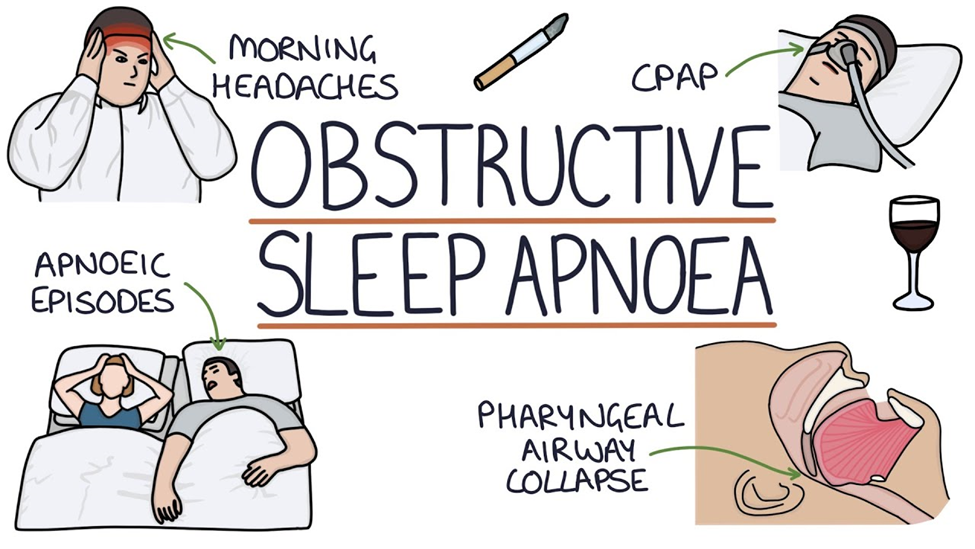
C. Headache
One of the common findings associated with obstructive sleep apnea (OSA) is headache. This occurs due to the repeated episodes of apnea (cessation of breathing) during sleep, which leads to intermittent hypoxia (low oxygen levels) and subsequent cerebral vasodilation. The vasodilation can trigger headaches, often described as morning headaches, upon waking up. These headaches are typically frontal and may be accompanied by other symptoms such as fatigue and irritability.
D. Hypotension
Hypotension (low blood pressure) is not a typical finding in obstructive sleep apnea. In fact, individuals with OSA are more likely to have hypertension (high blood pressure) due to the effects of repeated apnea episodes on the cardiovascular system, such as increased sympathetic activity and arterial stiffness.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
A. Auscultate breath sounds at least every 2 hours.
Regularly auscultating breath sounds is important for assessing respiratory status and detecting any signs of respiratory complications such as pneumonia or atelectasis. However, it is not the priority action in this scenario compared to applying antiembolic stockings, which directly addresses the increased risk of DVT and PE associated with immobility.
B. Perform range-of-motion exercises at least two to three times daily.
Range-of-motion exercises help prevent contractures and maintain joint mobility in immobile clients. While they are important for preventing musculoskeletal complications, they are not the priority action compared to applying antiembolic stockings, which directly addresses the increased risk of DVT and PE associated with immobility.
C. Make sure the client has an intake of 2,000 to 3,000 mL of fluid per day.
Maintaining adequate hydration is important for overall health and prevention of complications such as urinary tract infections and constipation. However, it is not the priority action in this scenario compared to applying antiembolic stockings, which directly addresses the increased risk of DVT and PE associated with immobility.
D. Apply antiembolic stockings.
The priority action for the nurse to contribute to the plan of care for an immobile client is to apply antiembolic stockings. Immobility increases the risk of deep vein thrombosis (DVT) and subsequent pulmonary embolism (PE). Antiembolic stockings (also known as compression stockings or TED stockings) help prevent venous stasis and decrease the risk of blood clots forming in the lower extremities. Therefore, applying antiembolic stockings is essential in mitigating the risk of potentially life-threatening complications associated with immobility.
Correct Answer is C
Explanation
A. Rest in a supine position.
This option is not recommended for improving gas exchange in emphysema. Resting in a supine position can lead to decreased lung expansion and increased dyspnea in individuals with emphysema. Optimal lung expansion is crucial for efficient gas exchange, and certain positions, such as sitting upright or using pillows to support the head and chest, are preferred to facilitate breathing.
B. Consume a low-protein diet.
A low-protein diet is not directly related to improving gas exchange in emphysema. In fact, adequate protein intake is important for maintaining overall health and supporting respiratory muscle function. Protein is necessary for tissue repair and maintaining muscle strength, including the respiratory muscles. Therefore, a balanced diet that includes adequate protein intake is recommended for individuals with emphysema.
C. Breathe in through her nose and out through pursed lips.
This is the correct choice. Breathing in through the nose and out through pursed lips helps to create positive pressure in the airways during exhalation. This positive pressure helps to keep the airways open, prevents premature collapse of the air sacs (alveoli), and facilitates more effective gas exchange. It also slows down the rate of breathing, reduces the work of breathing, and can alleviate shortness of breath (dyspnea) in individuals with emphysema.
D. Limit fluid intake throughout the day.
Limiting fluid intake throughout the day is not recommended for improving gas exchange in emphysema. Adequate hydration is important for thinning respiratory secretions, which can make it easier to clear mucus from the airways. Dehydration can worsen respiratory symptoms and increase the risk of complications. Therefore, maintaining adequate fluid intake is essential for individuals with emphysema.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
