A nurse is caring for a client with a medical diagnosis of acute exacerbation of chronic obstructive pulmonary disease (COPD). The client's assessment reveals a respiratory rate of 28/min, SpO2 at 90%, and complaints of mild dyspnea and anxiety at rest. What should the nurse include in the client's discharge teaching plan?
Use bronchodilators every 2 hours as needed.
Instructions on pursed-lip breathing.
Increase home oxygen from 3L/min to 5L/min as needed.
Use huff coughing to loosen secretions.
The Correct Answer is B
Choice A reason:
Using bronchodilators every 2 hours as needed may not be appropriate for all clients. Bronchodilators are typically used on a schedule or as needed based on symptoms, but overuse can lead to tolerance and decreased effectiveness. The nurse should provide education on the proper use and timing of bronchodilators.
Choice B reason:
Pursed-lip breathing is a technique that helps control shortness of breath and improve ventilation. It can slow down the client's breathing, promote relaxation, and ensure more effective lung function. This technique is particularly beneficial during an acute exacerbation of COPD and should be included in the discharge teaching plan.
Choice C reason:
Increasing home oxygen without proper assessment can be dangerous. Oxygen therapy should be titrated based on the client's oxygen saturation and clinical status. Clients with COPD are at risk of CO2 retention, and too much oxygen can suppress their drive to breathe. The nurse should educate the client on monitoring their SpO2 and when to adjust oxygen levels, typically under the guidance of a healthcare provider.
Choice D reason:
Huff coughing is a technique used to clear mucus from the airways. While it can be effective, it should be taught by a respiratory therapist or nurse who can assess the client's ability to perform the technique correctly. It is not the first-line teaching for a client being discharged with an acute exacerbation of COPD.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason
Using an antiemetic one hour after administration of methotrexate is not a standard recommendation. Antiemetics are typically used to prevent nausea and vomiting associated with chemotherapy and are taken before or at the time of methotrexate administration, not afterward.
Choice B Reason
Drinking 2-3 liters of water per day is important for patients taking methotrexate to prevent kidney damage by ensuring adequate hydration and facilitating the excretion of the drug¹. Methotrexate can be nephrotoxic, and proper hydration helps to mitigate this risk.
Choice C Reason
Rinsing the mouth with an alcohol-based mouthwash is not recommended for patients taking methotrexate. Alcohol can cause drying and irritation, which might exacerbate any mouth sores caused by methotrexate. Instead, patients should use a gentle, non-alcoholic mouthwash to maintain oral hygiene.
Choice D Reason
Taking methotrexate with an NSAID is not advised without specific medical guidance. NSAIDs can increase the toxicity of methotrexate by displacing it from protein-binding sites and reducing its renal clearance, potentially leading to increased side effects.
Correct Answer is C
Explanation
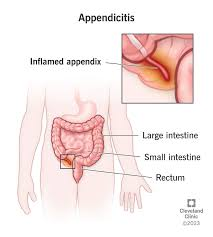
Choice A reason:
Offering a warm beverage to a client with suspected appendicitis is not advisable. Preoperative clients are typically required to have an empty stomach to reduce the risk of aspiration during anesthesia. Introducing fluids or food could delay surgery and increase the risk of complications.
Choice B reason:
Monitoring the client's gag reflex is not a priority in the care of a client with suspected appendicitis. The gag reflex is more relevant in neurological assessments or when evaluating swallowing function, not in the context of appendicitis.
Choice C reason:
Helping the client to a side-lying position with knees flexed can provide comfort and may help relieve abdominal pain. This position reduces tension on the abdominal muscles and can be a supportive measure while the client awaits surgery.
Choice D reason:
Applying a heating pad to the abdomen is contraindicated in clients with suspected appendicitis. Heat can cause the appendix to rupture, leading to peritonitis, which is a severe and potentially life-threatening complication. Therefore, this action should be avoided.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
