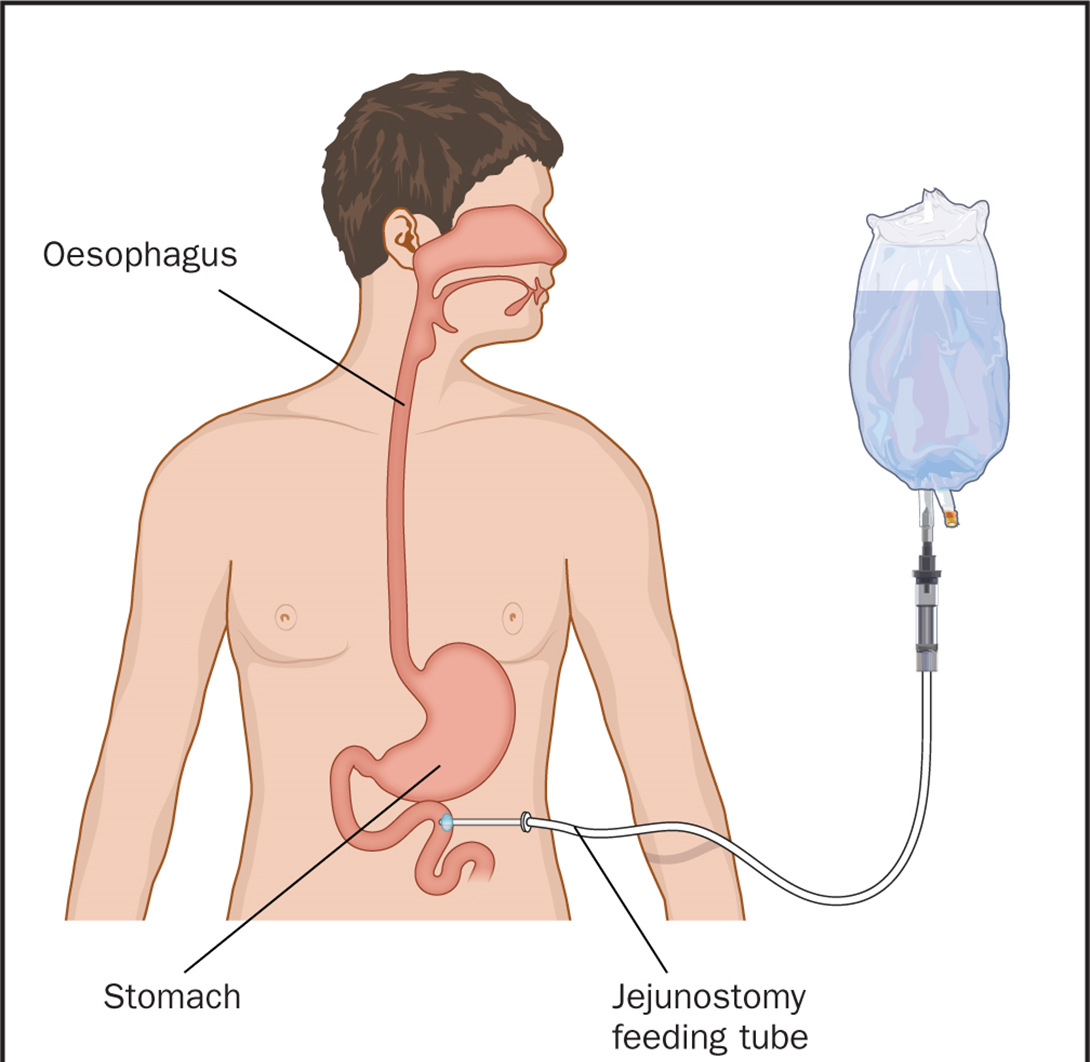
A nurse is caring for a client who has a gastrostomy tube and is receiving enteral nutrition. The nurse should identify that which of the following complications represents the greatest risk to the client?
Abdominal distention
Fluid overload
Glycosuria
Tube obstruction
The Correct Answer is D
Choice A reason: Abdominal distention is a possible complication of enteral nutrition, as it may indicate gas accumulation, constipation, or intolerance to the formula. However, it is not the greatest risk to the client, as it can be prevented or managed by adjusting the formula, rate, or volume of the feeding, or by administering medications or enemas.
Choice B reason: Fluid overload is a possible complication of enteral nutrition, as it may indicate excessive fluid intake, renal impairment, or heart failure. However, it is not the greatest risk to the client, as it can be prevented or managed by monitoring the fluid balance, electrolytes, and vital signs, or by administering diuretics or fluid restriction.
Choice C reason: Glycosuria is a possible complication of enteral nutrition, as it may indicate hyperglycemia, diabetes, or infection. However, it is not the greatest risk to the client, as it can be prevented or managed by monitoring the blood glucose, urine output, and signs of infection, or by administering insulin or antibiotics.
Choice D reason: Tube obstruction is the greatest risk to the client, as it may indicate clogging, kinking, or twisting of the tube, which can impair the delivery of the nutrition and medication, and cause aspiration, infection, or perforation. Tube obstruction can be prevented by flushing the tube with water before and after each feeding or medication, and by using a syringe or a pump to administer the formula. Tube obstruction can be managed by using warm water, carbonated beverages, or pancreatic enzymes to unclog the tube, or by replacing the tube if necessary.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A reason: Checking the client's deep tendon reflexes every 4 hr is a appropriate action for a nurse to take for a client who has hypomagnesemia. Hypomagnesemia is a low level of magnesium in the blood, which can cause neuromuscular excitability and hyperreflexia. The nurse should monitor the client's reflexes for signs of increased or decreased response, which can indicate worsening or improving hypomagnesemia.
Choice B reason: Encouraging the client to consume more fiber is not a relevant action for a nurse to take for a client who has hypomagnesemia. Fiber is beneficial for digestive health and blood glucose control, but it has no direct effect on magnesium levels. The nurse should encourage the client to consume foods that are rich in magnesium, such as green leafy vegetables, nuts, seeds, legumes, and whole grains.
Choice C reason: Restricting the client's fluid intake to 500 mL/day is not a safe or effective action for a nurse to take for a client who has hypomagnesemia. Fluid restriction can cause dehydration, electrolyte imbalance, and kidney damage, which can worsen hypomagnesemia. The nurse should maintain the client's fluid balance and monitor their urine output and specific gravity.
Choice D reason: Limiting sodium-containing foods on the client's meal tray is not a necessary action for a nurse to take for a client who has hypomagnesemia. Sodium is not directly related to magnesium levels, and limiting sodium intake can cause hyponatremia, which is a low level of sodium in the blood. The nurse should ensure that the client receives adequate sodium intake from their diet or supplements.
Correct Answer is B
Explanation
Choice A reason: Diabetes mellitus is not a likely complication of malnutrition, as it is caused by insufficient insulin production or action, not by inadequate food intake. Malnutrition may worsen the outcomes of diabetes, but it does not cause it.
Choice B reason: Pressure injury is a common complication of malnutrition, as it is caused by impaired tissue perfusion and oxygenation due to poor nutrition. Malnutrition can lead to loss of muscle mass, subcutaneous fat, and skin integrity, which increase the risk of developing pressure ulcers.
Choice C reason: Heat intolerance is not a direct complication of malnutrition, as it is caused by impaired thermoregulation due to hormonal or neurological disorders, not by insufficient food intake. Malnutrition may affect the body's ability to cope with heat stress, but it does not cause it.
Choice D reason: Gastroesophageal reflux disease (GERD) is not a typical complication of malnutrition, as it is caused by the backflow of gastric contents into the esophagus due to a weak or incompetent lower esophageal sphincter, not by inadequate food intake. Malnutrition may aggravate the symptoms of GERD, but it does not cause it.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
