A nurse is caring for a client who has a central venous catheter and suddenly develops chest pain, dyspnea, dizziness, and tachycardia. The nurse suspects air embolism and clamps the catheter immediately. What other action should the nurse take at this time?
Remove the catheter.
Replace the infusion system.
Prepare for chest tube insertion.
Place the client on his left side in Trendelenburg position.
The Correct Answer is D
A. Remove the catheter: Removing the catheter may not be the immediate priority. The nurse should focus on preventing further air entry into the circulation and addressing the symptoms.
B. Replace the infusion system: While ensuring that the infusion system is intact is important, it is not the primary action needed to manage an air embolism.
C. Prepare for chest tube insertion: Chest tube insertion is not the primary intervention for an air embolism. The focus should be on preventing the progression of the embolism and providing supportive care.
D. Place the client on his left side in Trendelenburg position: This is the correct answer. Placing the client on the left side in Trendelenburg position is a maneuver used to trap air in the right atrium, preventing it from traveling to the pulmonary artery. The left side position helps to prevent the air from traveling to the right ventricle and into the pulmonary artery, reducing the risk of further complications.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
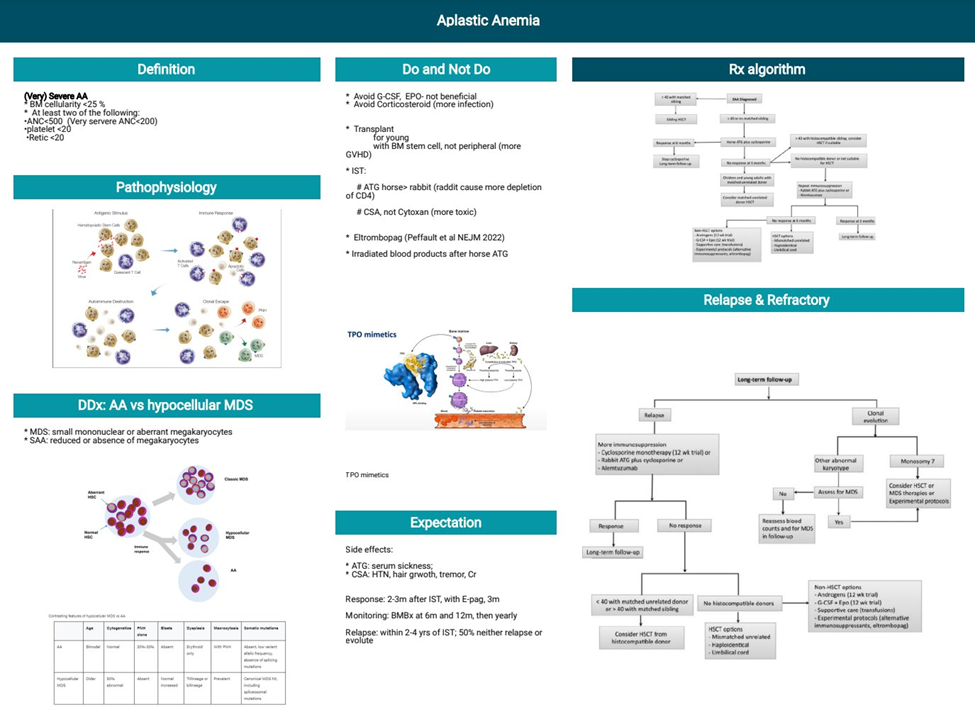
A. Aplastic anemia results in an inability to absorb vitamin B12: This statement is incorrect. Aplastic anemia is not related to the absorption of vitamin B12. It primarily involves a decrease in the production of blood cells by the bone marrow.
B. Aplastic anemia results from decreased bone marrow production of RBCs: This is the correct information. Aplastic anemia is a condition characterized by the failure of the bone marrow to produce an adequate number of blood cells, including red blood cells (RBCs), white blood cells (WBCs), and platelets.
C. Aplastic anemia results in an increased rate of RBC destruction: This statement is incorrect. Aplastic anemia is not associated with an increased rate of RBC destruction. Instead, it is characterized by a reduction in the number of blood cells produced by the bone marrow.
D. Aplastic anemia is associated with a decreased intake of iron: This statement is incorrect. Aplastic anemia is not related to a decreased intake of iron. It is primarily a disorder of bone marrow function leading to insufficient production of blood cells.
Correct Answer is B
Explanation
A. Myringotomy: Myringotomy is a procedure involving the insertion of tubes into the eardrum to treat conditions such as chronic ear infections. This procedure is not associated with a significant risk of deep-vein thrombosis.
B. Hip arthroplasty: Hip arthroplasty, or hip replacement surgery, is associated with an increased risk of deep-vein thrombosis due to factors such as immobility, surgical trauma, and alterations in blood flow. Prophylactic measures, such as anticoagulant medications and early ambulation, are often employed to reduce this risk.
C. Cataract extraction: Cataract extraction is a procedure to remove a cloudy lens from the eye. This surgery is not typically associated with a high risk of deep-vein thrombosis.
D. Laparoscopic appendectomy: Laparoscopic appendectomy, a minimally invasive procedure to remove the appendix, is generally associated with a lower risk of deep-vein thrombosis compared to major orthopedic surgeries like hip arthroplasty.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
