A nurse is attending a social event when another guest coughs weakly once, grasps his throat with his hands, and cannot talk. Which of the following actions should the nurse take?
Perform the Heimlich maneuver.
Slap the client on the back several times.
Assist the client to the floor and begin mouth-to-mouth resuscitation.
Observe the client before taking further action.
The Correct Answer is A
Choice A reason:
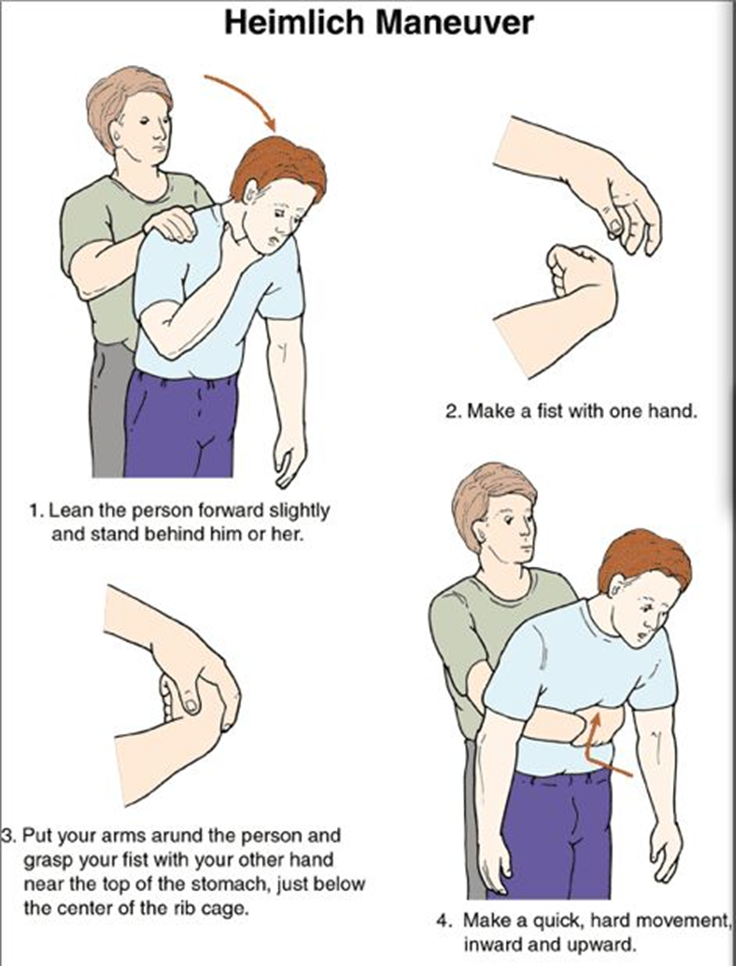
The Heimlich maneuver, also known as abdominal thrusts, is the recommended first aid technique for a conscious person who is choking. This maneuver helps to expel the object blocking the airway by using the air remaining in the lungs to force it out. The nurse should stand behind the person, place their arms around the person’s waist, make a fist with one hand, and place it just above the navel. The other hand should grasp the fist, and quick, upward thrusts should be performed until the object is expelled.
Choice B reason:
Slapping the client on the back several times is not the recommended first action for a conscious adult who is choking. While back blows can be effective, they are typically used in combination with abdominal thrusts and are more commonly recommended for infants. For adults, the Heimlich maneuver is preferred as the initial response.
Choice C reason:
Assisting the client to the floor and beginning mouth-to-mouth resuscitation is not appropriate for a conscious person who is choking. Mouth-to-mouth resuscitation, or rescue breathing, is used when a person is not breathing and is unresponsive. In this scenario, the client is conscious but unable to speak, indicating a blocked airway that requires the Heimlich maneuver.
Choice D reason:
Observing the client before taking further action is not advisable in a choking emergency. Immediate intervention is crucial to prevent the situation from worsening. If the person is unable to speak, cough, or breathe, the Heimlich maneuver should be performed without delay.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A reason: The Health Care Proxy Does Not Go Into Effect Until I Am Incapable of Making Decisions
This statement is correct. A health care proxy, also known as a durable power of attorney for health care, only becomes active when the individual is no longer capable of making their own medical decisions. Until that point, the individual retains full control over their health care choices1.
Choice B reason: I Have to Choose a Family Member as My Health Proxy
This statement indicates a need for clarification. It is not necessary to choose a family member as a health care proxy. An individual can select any trusted person, whether a family member or a friend, to act as their health care proxy. The most important factor is that the chosen person understands the individual’s wishes and is willing to advocate for them2.
Choice C reason: I Can Change Who I Designate as My Health Care Proxy at Any Time
This statement is correct. An individual can change their designated health care proxy at any time, as long as they are still capable of making their own decisions. It is important to ensure that any changes are documented properly and that all relevant parties are informed of the change3.
Choice D reason: If I Become Incapacitated, End-of-Life Choices Will Be Made by My Proxy
This statement is correct. If an individual becomes incapacitated and is unable to make their own medical decisions, the health care proxy will step in to make decisions on their behalf, including end-of-life choices. The proxy should be well-informed about the individual’s preferences and values to make decisions that align with their wishes4.
Correct Answer is C
Explanation
Choice A reason:
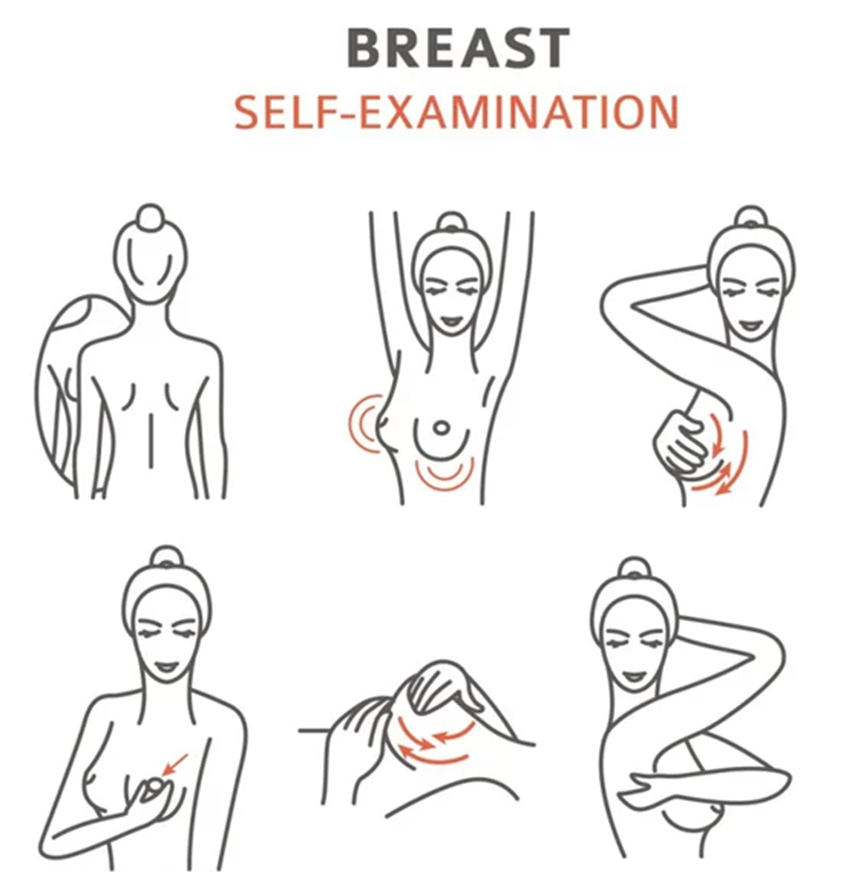
Using the palm of the hand, feel for lumps using a circular motion: This instruction is incorrect. The correct method for a breast self-exam involves using the pads of the three middle fingers, not the palm of the hand. The fingers should move in a circular motion to feel for lumps or abnormalities.
Choice B reason:
Expect some breast dimpling or discharge with age: This is misleading and potentially harmful advice. While some changes in the breast can occur with age, dimpling or discharge can also be signs of breast cancer and should be reported to a healthcare provider immediately.
Choice C reason:
Breasts can be examined in the shower with soapy hands: This is correct. Examining the breasts in the shower with soapy hands can make it easier to feel for lumps or changes. The soapy water helps the fingers glide smoothly over the skin, making it easier to detect any abnormalities.
Choice D reason:
For those who have a menstrual cycle, perform a BSE every month, 2 or 3 days before menstruation: This instruction is incorrect. The best time to perform a breast self-exam is a few days after the menstrual period ends, when the breasts are least likely to be swollen or tender.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
