A nurse is assisting with the admission of an older adult client who has impaired mobility and is at risk for falls. Which of the following actions should the nurse plan to perform first?
Check the client's ability to use the call light.
Document the client's risk in the medical record.
Request a referral for physical therapy
Place a gait belt in the client's room.
The Correct Answer is A
The first action the nurse should plan to perform is to check the client's ability to use the call light. This is essential to ensure that the client can easily communicate with the healthcare team if they need assistance or experience a fall risk situation. By confirming the client's ability to use the call light, the nurse can address any potential communication barriers and ensure that the client has a means to request help promptly.
Explanation for the other options:
b) Document the client's risk in the medical record: While documenting the client's risk in the medical record is important, it is not the first action to be taken. Ensuring the client's immediate safety and ability to request assistance is the priority.
c) Request a referral for physical therapy: Referring the client for physical therapy may be a necessary step to address their impaired mobility and reduce fall risk, but it is not the first action to be performed. Assessing their ability to use the call light takes precedence in order to address immediate safety concerns.
d) Place a gait belt in the client's room: Providing a gait belt is a measure to assist with mobility and falls prevention. However, it should not be the first action. Checking the client's ability to use the call light is more critical to ensure their immediate safety and ability to request help.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
b. Give directions using simple phrases.
The correct answer is b. Give directions using simple phrases.
Explanation:
When assisting with the plan of care for a client with Alzheimer's disease, it is important to consider their cognitive impairments and provide appropriate interventions. Giving directions using simple phrases is recommended because it helps the client beter understand and follow instructions. Complex or lengthy directions can be confusing and overwhelming for individuals with Alzheimer's disease. Using clear and concise language can enhance communication and facilitate the client's ability to engage in activities of daily living.
Explanation for the other options:
a. Encourage the client to talk about current events: While social interaction and engagement are beneficial for clients with Alzheimer's disease, their ability to comprehend and discuss current events may be limited due to cognitive impairments. It is important to adapt communication to the client's cognitive abilities and interests.
c. Orient the client to time and place twice per day: Frequent orientation to time and place can be helpful for clients with Alzheimer's disease, but the specific frequency should be based on the individual's needs and preferences. Some individuals may require more frequent orientation, while others may find it overwhelming. The plan of care should be individualized to address the client's specific needs.
d. Rotate assistive personnel to help the client with ADLs: Consistency and familiarity are important for individuals with Alzheimer's disease. Rotating assistive personnel frequently may disrupt the client's routine and cause increased confusion and agitation. Whenever possible, it is best to maintain a consistent caregiving team to provide familiarity and establish a therapeutic relationship with the client.
In summary, giving directions using simple phrases is an appropriate action when assisting with the plan of care for a client with Alzheimer's disease. This approach promotes effective communication and enhances the client's ability to understand and follow instructions.

Correct Answer is C
Explanation
The correct answer and explanation is:
c. Denial
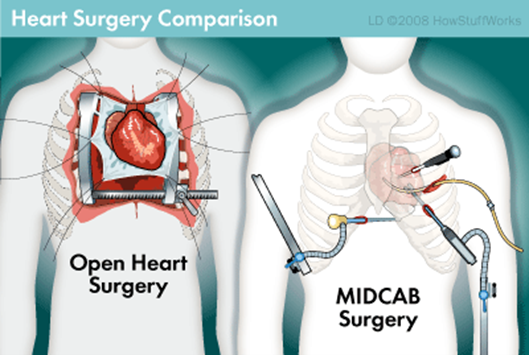
The nurse should identify that the client is experiencing the stage of denial in the grief process. Denial is a common psychological defense mechanism that individuals may exhibit when faced with a stressful or overwhelming situation, such as the prospect of open heart surgery. It involves a refusal to accept or acknowledge the reality of the situation. In this case, the client's statement of being confident to go home shortly after surgery demonstrates a denial of the potential challenges and recovery process associated with such a procedure.
Explanation for the other options:
A . Anger: Anger is a stage of grief characterized by feelings of resentment, frustration, and hostility. It is common for individuals to experience anger as part of the grief process, but the client's statement does not indicate anger.
B. Depression: Depression is another stage of grief marked by feelings of sadness, hopelessness, and loss. While it is normal for individuals to experience some level of anxiety or sadness before undergoing surgery, the client's statement does not specifically reflect depression.
d. Acceptance: Acceptance is the final stage of grief, where individuals come to terms with their situation and find a sense of peace or resolution. The client's statement indicates a lack of acceptance as they are denying the potential impact of the surgery and its recovery process.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
