A nurse is assessing an older adult client who has dysphagia and is experiencing dehydration. Which of the following findings should the nurse expect?
Tachycardia
Hypertension
Distended neck veins
Decreased respiratory rate
The Correct Answer is A
The expected finding in an older adult client with dysphagia and dehydration is tachycardia. Tachycardia, an increased heart rate, is a common finding in dehydration as the body tries to compensate for the decreased fluid volume.
The other choices (hypertension, distended neck veins, and decreased respiratory rate) are not typically associated with dehydration in this context.
here's an explanation of why these choices are incorrect:
1. Hypertension: Dehydration usually leads to a decrease in blood volume, resulting in low blood pressure rather than hypertension. Hypertension is not a typical finding in dehydration.
2. Distended neck veins: Dehydration causes a decrease in blood volume, which results in decreased venous return to the heart. Consequently, distended neck veins would not be an expected finding.
3. Decreased respiratory rate: Dehydration itself does not directly affect respiratory rate. However, severe dehydration can lead to electrolyte imbalances, such as hyponatremia (low sodium levels), which can affect brain function and potentially lead to changes in respiratory rate. However, decreased respiratory rate is not a common finding in dehydration alone.
It's important to remember that dehydration can have various signs and symptoms, including dry mucous membranes, decreased urine output, increased thirst, dry skin, dizziness, and confusion.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Place the client in a semi-Fowler's position when eating. The semi-Fowler's position involves elevating the head of the bed to an angle of 30 to 45 degrees. This position helps prevent aspiration by facilitating proper swallowing and reducing the risk of food or liquid entering the airway.

Initiating a calorie count of daily food intake is not a specific action for dysphagia. Calorie counting is generally used for monitoring caloric intake in clients with specific dietary needs or conditions, but it is not directly related to dysphagia management. The focus for dysphagia management is on ensuring safe swallowing and preventing complications such as aspiration.
Instructing the client to keep their chin up when swallowing is not appropriate for dysphagia management. This action can actually increase the risk of aspiration. The proper technique for swallowing with dysphagia typically involves tucking the chin slightly down towards the chest to help close off the airway and direct the food or liquid down the esophagus.
Providing food in a thin liquid consistency is not appropriate for dysphagia unless specifically recommended by a healthcare professional. Dysphagia diets typically involve modifying the consistency of food and liquids based on the client's swallowing abilities and recommendations from a speech-language pathologist or dietitian. Different levels of texture modifications (such as pureed, minced, or mechanically soft) may be prescribed to ensure safe swallowing and reduce the risk of aspiration.
Correct Answer is A
Explanation
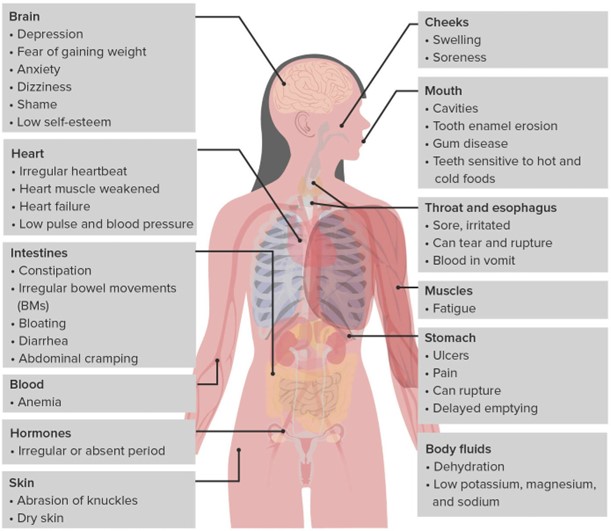
Low potassium levels, known as hypokalemia, can be a significant concern in individuals with bulimia nervosa due to the frequent purging behaviors associated with the condition. Purging, such as self-induced vomiting or misuse of laxatives or diuretics, can lead to excessive loss of potassium from the body. Hypokalemia can have serious consequences, including cardiac arrhythmias, muscle weakness, fatigue, and even life-threatening complications.
The normal range for potassium is typically around 3.5-5.0 mEq/L. With a potassium level of 3.2 mEq/L falling below the normal range, it indicates a low potassium level and requires prompt attention.
The other laboratory results mentioned in the question are within normal ranges:
● A WBC (white blood cell) count of 5,200/mm3 falls within the normal range (typically between 4,500 and 11,000/mm3) and indicates a normal white blood cell count.
● An Hgb (hemoglobin) level of 14 g/dL falls within the normal range (typically between 12 and 16 g/dL) and indicates a normal hemoglobin level.
● A magnesium level of 1.6 mEq/L, although slightly low, is still within the normal range (typically between 1.5 and 2.5 mEq/L). The nurse should monitor it closely and assess for symptoms associated with hypomagnesemia. If the client's symptoms or other clinical indications suggest a significant magnesium imbalance, the healthcare provider should be notified.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
