A nurse is assessing a full-term newborn. Which of the following findings should the nurse report to the provider?
Respiratory rate 55/min
Blood pressure 80/50 mm Hg
Temperature 36.5°C (97.7°F)
Heart rate 72/min
The Correct Answer is D
Heart rate is one of the vital signs that reflects the health and well-being of a newborn. It is measured by counting the number of heart beats per minute, either by listening to the chest with a stethoscope or by feeling the pulse at the wrist, elbow, or groin. Heart rate can vary depending on the newborn's activity level, temperature, and emotional state¹.
The normal range for heart rate in full-term newborns is 120 to 160 beats per minute. The heart rate may be slightly higher or lower depending on the newborn's age, weight, and gestational age. For example, premature newborns may have a higher heart rate than term newborns, and heavier newborns may have a lower heart rate than lighter newborns¹².
A heart rate that is too high (tachycardia) or too low (bradycardia) can indicate a problem with the newborn's heart function, oxygenation, or circulation. Some of the possible causes of abnormal heart rate in newborns are:
- Congenital heart defects: structural abnormalities of the heart that are present at birth and affect the blood flow through the heart and the body. They can cause cyanosis (bluish skin color), murmur (abnormal heart sound), poor feeding, or failure to thrive¹³.
- Arrhythmias: irregular or abnormal heart rhythms that can affect the electrical impulses that control the heartbeat. They can cause palpitations (feeling of skipped or extra beats), dizziness, fainting, or cardiac arrest¹³.
- Hypoxia: lack of oxygen in the blood or tissues that can affect the brain and other organs. It can be caused by respiratory distress, anemia, infection, or birth asphyxia. It can cause bradycardia, apnea (pauses in breathing), seizures, or coma¹⁴.
- Hypothermia: low body temperature that can affect the metabolism and organ function. It can be caused by exposure to cold environment, infection, or prematurity. It can cause bradycardia, lethargy, poor feeding, or hypoglycemia (low blood sugar)¹⁴.
- Sepsis: severe infection that can affect the whole body and cause inflammation and organ damage. It can be caused by bacteria, viruses, fungi, or parasites that enter the bloodstream from the mother, the umbilical cord, or the environment. It can cause tachycardia, fever, chills, poor feeding, or shock¹⁴.
Therefore, the nurse should report a heart rate of 72/min to the provider as an abnormal finding and monitor the newborn for any other signs of distress or illness. The provider may order further tests or treatments to determine the cause and severity of the low heart rate and prevent any complications.
The other findings are not findings that the nurse should report to the provider because they are within the
normal range for full-term newborns:
- a) Respiratory rate 55/min is within the normal range for respiratory rate in full-term newborns. The normal range for respiratory rate in full-term newborns is 40 to 60 breaths per minute. The respiratory rate may vary depending on the newborn's activity level, temperature and emotional state¹².
- b) Blood pressure 80/50 mm Hg is within the normal range for blood pressure in full-term newborns. The normal range for blood pressure in full-term newborns is 65 to 95 mm Hg for systolic pressure (the top number) and 30 to 60 mm Hg for diastolic pressure (the bottom number). The blood pressure may vary depending on the newborn's age, weight, and gestational age¹².
- c) Temperature 36.5°C (97.7°F) is within the normal range for temperature in full-term newborns. The normal range for temperature in full-term newborns is 36.5°C to 37.5°C (97.7°F to 99.5°F). The temperature may vary depending on the newborn's activity level, clothing, and environment¹².
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
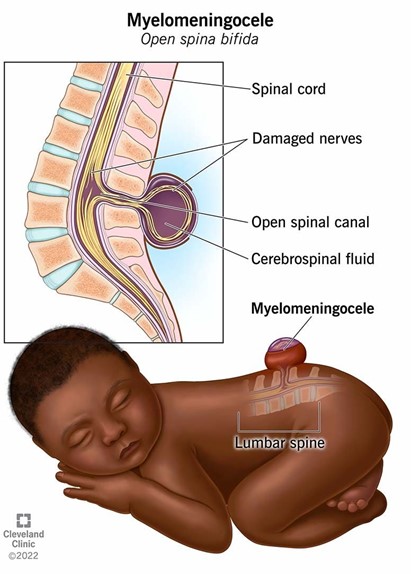
A. Using povidone-iodine on the site of a myelomeningocele is not recommended as it can be irritating to the tissue and might not be safe for use on open neural tissue. The focus should be on preventing infection through other means.
B. Administering broad-spectrum antibiotics is crucial as the cerebrospinal fluid (CSF) leak increases the risk of infection, such as meningitis. Antibiotics help protect the newborn from potentially serious infections until surgical repair can be performed.
C. Surgical closure of a myelomeningocele is typically done as soon as possible, often within 24-48 hours after birth, to minimize the risk of infection and further damage to the exposed spinal cord.
D. While monitoring temperature is important, rectal temperature measurement is not recommended for a newborn with a myelomeningocele due to the risk of causing further complications. Axillary temperature measurement would be safer and less invasive.
Correct Answer is A
Explanation
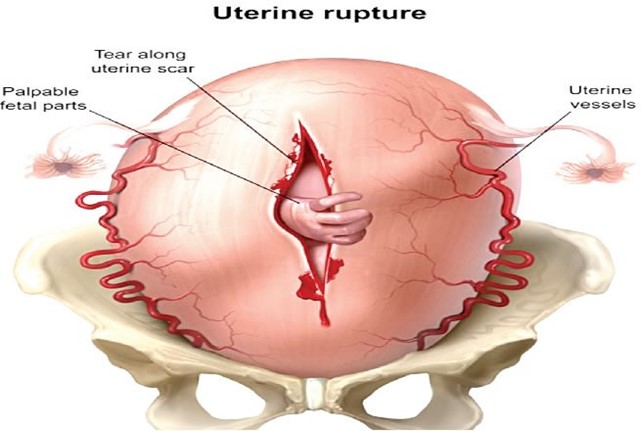
Uterine rupture is a rare but life-threatening complication of labor and delivery that occurs when the uterus tears open along the scar line of a previous cesarean delivery or other uterine surgery¹². Uterine rupture can cause severe bleeding in the mother and deprive the baby of oxygen¹². Some of the signs and symptoms of uterine rupture are:
- Sudden, severe lower abdominal pain
- Drop in blood pressure
- Cool skin and pallor
- Prolonged fetal bradycardia (slow heart rate)
- Loss of fetal station (the baby moves back up the birth canal)
- Abnormal or absent uterine contractions¹²³
Uterine rupture is a medical emergency that requires immediate surgery to deliver the baby and repair the uterus or remove it (hysterectomy)¹².
The other options are incorrect because they have different signs and symptoms:
b) Amniotic fluid embolism is a rare but serious condition that occurs when amniotic fluid or fetal cells enter the mother's bloodstream and trigger an allergic reaction. It can cause sudden respiratory distress, cardiac arrest, seizures, or coma in the mother and fetal distress or death in the baby¹². It usually occurs during labor, delivery, or shortly after birth¹².
c) Placenta previa is a condition where the placenta covers part or all of the opening of the cervix. It can cause painless vaginal bleeding during pregnancy or labor¹². It does not affect the blood pressure or fetal heart rate unless there is severe bleeding or placental abruption (separation of the placenta from the uterine wall)¹².
d) Umbilical cord prolapse is a condition where the umbilical cord slips through the cervix and into the vagina before or during labor. It can cause fetal distress, as the cord can become compressed or twisted, cutting off the blood supply and oxygen to the baby¹². It usually causes a sudden drop in fetal heart rate, but does not affect the maternal blood pressure or cause abdominal pain¹².
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
