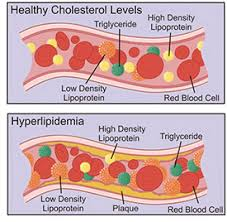
A nurse is assessing a client who has been taking simvastatin to treat hyperlipidemia. Which statement made by the client describes an adverse effect of the medication that should be reported to the provider immediately?
"I've had gas pains for the last day."
"I've had a headache for a couple of days."
"I have occasional constipation."
"My legs feel weak, and I get pain in my calves."
The Correct Answer is D
Choice A Reason:
Gas pains, while uncomfortable, are not typically a serious adverse effect of simvastatin and do not usually require immediate medical attention unless they are severe or persistent.
Choice B Reason:
Headaches are a common side effect of many medications, including simvastatin, and are not generally considered an emergency. However, if the headache is severe, persistent, or accompanied by other symptoms, it should be reported to a healthcare provider.
Choice C Reason:
Occasional constipation is another common side effect and is not usually a cause for immediate concern unless it becomes severe or chronic.
Choice D Reason:
Muscle weakness and pain, especially in the calves, can be a sign of a serious condition called rhabdomyolysis, which is a rare but serious adverse effect of statins like simvastatin. This condition involves the breakdown of muscle tissue and can lead to kidney damage. It should be reported to a healthcare provider immediately.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
Switching to heparin is not the standard response for a high INR. Heparin may be used in conjunction with warfarin when starting anticoagulation therapy, but it is not typically used as a substitute in response to an elevated INR.
Choice B Reason:
Giving the dose as prescribed would not be appropriate when the INR is significantly above the therapeutic range. Continuing the same dose could increase the risk of bleeding complications.
Choice C Reason:
Increasing the dose would be contraindicated as the INR is already too high. Increasing the warfarin dose would further elevate the INR and increase the risk of bleeding.
Choice D Reason:
Holding the dose is the correct action when the INR is significantly above the therapeutic range, which is generally between 2.0 to 3.0 for most indications. The healthcare provider should be notified, and the warfarin dose should be held until the INR returns to the therapeutic range. Vitamin K may also be administered to help lower the INR more quickly if necessary.
Correct Answer is D
Explanation
Choice A reason:
Administering oxygen using a non-rebreather mask is a subsequent step if initial measures do not improve fetal heart rate decelerations. It can help increase the amount of oxygen available to the fetus. Oxygen administration is a supportive measure that can be used if there are signs of fetal distress. In the scenario described, where the fetal heart rate slows after the start of a contraction with the lowest rate occurring after the peak, it suggests late decelerations, which are often associated with uteroplacental insufficiency. Administering oxygen can help increase the fetal oxygen reserve and is a common intervention during labor when there are concerns about fetal well-being.
Choice B reason:
Increasing the rate of maintenance IV infusion is typically considered when there is a concern for maternal hypotension or dehydration, which may not be the immediate cause of the observed fetal heart rate pattern. Increasing the rate of an IV infusion can help improve maternal hydration and blood pressure, which in turn can enhance placental perfusion. However, this intervention is more indirect and may not provide the immediate response needed to address fetal heart rate decelerations. It is typically considered after more direct interventions, such as repositioning the mother, have been attempted.
Choice C reason:
Elevating the client's legs can help improve venous return to the heart, potentially increasing maternal cardiac output and blood flow to the placenta. While this can be beneficial, it is not the primary intervention for late decelerations. Repositioning the mother to improve uteroplacental circulation is generally the first step.
Choice D reason:
Placing the client in the lateral position is often the first action taken when late decelerations are observed. This position helps improve uteroplacental blood flow and can quickly address potential issues related to fetal oxygenation. This position helps to relieve pressure on the inferior vena cava and aorta, which can be compressed by the gravid uterus, especially in the supine position. Relieving this pressure helps to improve uteroplacental circulation and can quickly address the cause of late decelerations, which is often related to compromised blood flow to the placenta.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
