A nurse in a PACU is transferring care of a client to a nurse on the medical-surgical unit.
Which of the following statements should the nurse include in the hand-off report?
“The client was intubated without complications.”
“There was a total of 10 sponges used during the procedure.”
“The estimated blood loss was 250 milliliters.”
“The client is a member of the board of directors.”.
The Correct Answer is C
This statement should be included in the hand-off report because it provides essential information about the patient’s intraoperative status and potential postoperative complications, such as hypovolemia, anemia, or infection. The estimated blood loss (EBL) is an important indicator of the patient’s fluid balance and hemodynamic stability.
Choice A is wrong because “The client was intubated without complications.” is not relevant for the postoperative care of the patient. The intubation status is usually documented in the anesthesia record and does not need to be repeated in the hand-off report unless there were any issues or injuries related to the airway management.
Choice B is wrong because “There was a total of 10 sponges used during the procedure.” is not pertinent for the postoperative care of the patient.
The number of sponges used during the surgery is usually counted and verified by the scrub nurse and the circulating nurse in the operating room to prevent any retained foreign bodies. This information does not need to be communicated to the PACU nurse unless there was a discrepancy or a missing sponge.
Choice D is wrong because “The client is a member of the board of directors.” is not appropriate for the hand-off report.
This statement violates the patient’s privacy and confidentiality and does not contribute to the quality or safety of care. The patient’s role or position in the organization should not influence the hand-off communication or the postoperative care.
A hand-off report is a critical communication tool that facilitates the transfer of care from one provider to another. It should include relevant information about the patient’s medical history, surgical procedure, intraoperative events, postoperative plan, and any concerns or potential problems.
A standardized hand-off tool, such as SBAR (Situation, Background, Assessment, Recommendation), can help improve the consistency, accuracy, and completeness of the hand-off report.
Some normal ranges that may be useful for postoperative care are:
- Blood pressure: 90/60 mmHg to 120/80 mmHg
- Pulse: 60 to 100 beats/min
- Respiratory rate: 12 to 20 breaths/min
- Oxygen saturation: 95% to 100%
- Temperature: 36°C to 37.5°C
- Hemoglobin: 12 to 18 g/dL
- Hematocrit: 36% to 54%
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A reason
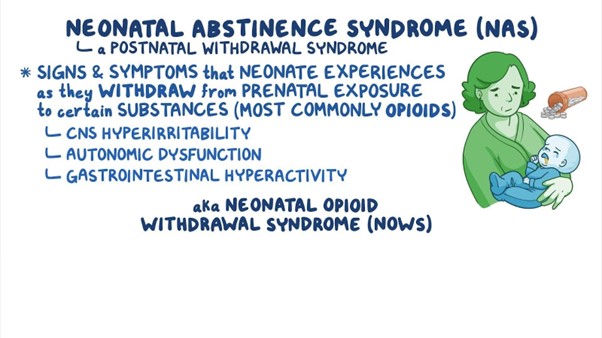
Administering naloxone to the newborn is not appropriate. Naloxone is an opioid antagonist used to reverse the effects of opioid overdose in adults. It is not typically used for newborns with neonatal abstinence syndrome. The management of NAS is primarily supportive, and medications may be prescribed to help manage specific withdrawal symptoms, but naloxone is not a standard treatment for NAS.
Choice B reason:
Minimizing noise in the newborn's environment is a crucial action in the plan of care is the correct action to be included. Newborns experiencing NAS can be easily overstimulated, and loud noises can exacerbate their withdrawal symptoms and distress. Creating a calm and quiet environment helps reduce agitation and promotes better sleep and overall comfort.
Choice C reason
Swaddling the newborn with his leg extended is not appropriate in this case. Swaddling can be beneficial for some newborns, but the specific positioning and swaddling techniques should be individualized based on the newborn's needs and preferences. Extending the newborn's legs may not necessarily be the best approach, as it may not provide comfort or address the symptoms associated with NAS.
Choice D reason:
Maintaining eye contact with the newborn during feedings is not appropriate in this case. While maintaining eye contact during feedings is an essential aspect of bonding and promoting parent-newborn attachment, it may not be the primary focus in managing neonatal abstinence syndrome. The plan of care for a newborn with NAS would primarily involve managing withdrawal symptoms, providing comfort measures, and addressing the newborn's unique needs during this challenging period.
Correct Answer is D
Explanation
The correct answer is choice D. The nurse should choose a vein that is palpable and straight for IV catheter insertion.
This will facilitate the insertion of the catheter and reduce the risk of complications such as infiltration, phlebitis, or hematoma. A straight vein will also allow the catheter to be inserted up to the hub, which reduces the risk of contamination along the length of the catheter.
Choice A is wrong because selecting a site on the client’s dominant arm can interfere with the client’s mobility and increase the risk of dislodging the catheter. The nurse should choose a site on the client’s non-dominant arm, preferably on the hand or forearm.
Choice B is wrong because applying a tourniquet below the venipuncture site will impede blood flow and make it harder to locate a suitable vein. The nurse should apply a tourniquet above the venipuncture site, about 10 to 15 cm from the insertion site.
Choice C is wrong because elevating the client’s arm prior to insertion will decrease venous filling and make it harder to palpate a vein. The nurse should lower the client’s arm below the level of the heart to increase venous distension.
Normal ranges for IV catheter size and insertion angle depend on several factors, such as the type and duration of therapy, the condition and size of the vein, and the age and preference of the client.
In general, smaller gauge catheters (20 to 24) are preferred for peripheral IV therapy, and larger gauge catheters (14 to 18) are used for rapid fluid administration or blood transfusion. The insertion angle can vary from 10 to 30 degrees, depending on the depth and location of the vein.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
