A client whose first child was delivered by cesarean section is 20 weeks pregnant with her second child and wishes to have a vaginal birth after cesarean (VBAC). What information is most important for the practical nurse (PN) to obtain?
Client's intent regarding breastfeeding of the newborn.
The type of uterine incision used for previous birth.
History of contracting Herpes simplex virus.
Religious preference of the client's family.
The Correct Answer is B
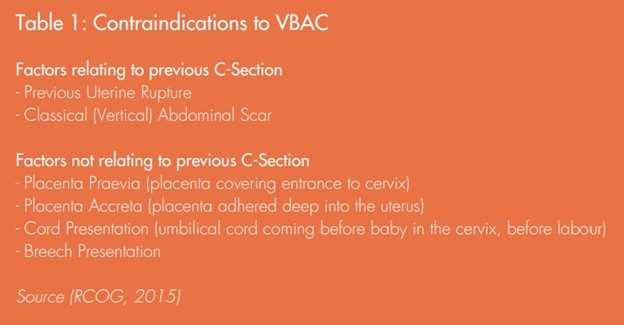
Knowing the type of uterine incision from the previous cesarean section is crucial when considering the option of vaginal birth after cesarean (VBAC). The type of incision can provide important insights into the potential risks and complications associated with a trial of labor.
Specifically, a low transverse uterine incision is considered the most favorable for VBAC, as it has a lower risk of uterine rupture compared to other types of incisions, such as a classical or vertical incision.
A. While information about the client's intent regarding breastfeeding of the newborn is important for providing appropriate support and education, it does not have a direct impact on the decision-making process for VBAC.
C. A history of contracting Herpes simplex virus is relevant to the client's overall health and may have implications for the management of the pregnancy, but it is not directly related to the decision regarding VBAC.
D. The religious preference of the client's family, while important for respecting cultural and spiritual beliefs, does not have a direct impact on the decision-making process for VBAC.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
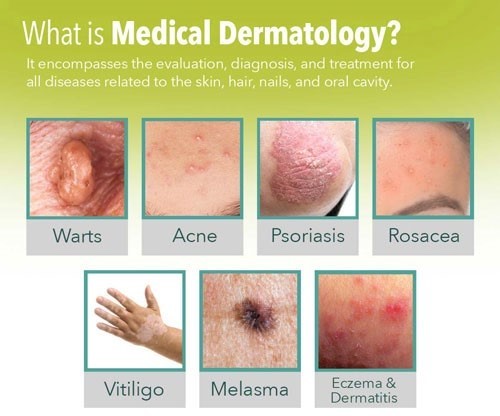
Acne is a common skin condition that often requires specialized treatment. While general skin care practices can help maintain healthy skin, the most appropriate recommendation for a 16-year-old client seeking treatment for acne is to refer them to a dermatologist.
Acne can have various underlying causes, and effective treatment often involves a tailored approach based on the individual's specific condition. Dermatologists are medical professionals specializing in skin health and are best equipped to assess and provide appropriate treatment options for acne.
Correct Answer is B
Explanation
In infants with heart failure, they may have difficulty feeding due to fatigue and increased work of breathing. Allowing the infant to rest before feeding helps conserve their energy and reduces the risk of excessive fatigue during feeding.
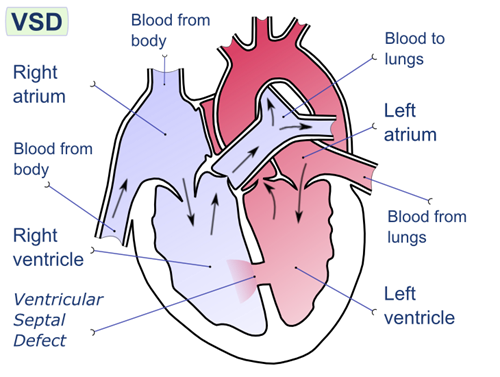
The other options are not appropriate interventions for this situation:
A.Weigh before and after feeding: Weighing before and after feeding is not necessary in this case unless specifically ordered by the healthcare provider. It is not directly related to the management of feeding an infant with heart failure.
C.Feed the infant when he cries: Feeding the infant solely based on crying may not be appropriate in this case. It is important to establish a feeding schedule and monitor the infant's signs of hunger and satiety to ensure adequate nutrition and prevent overfeeding.
D.Insert a nasogastric feeding tube: Inserting a nasogastric feeding tube should not be the first intervention unless there is a specific indication or order from the healthcare provider. In this scenario, the focus is on supporting oral feeding and allowing the infant to rest before feeding.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
