A client receiving mechanical ventilation has a pH of 7.26, PaCO2 of 68 mm Hg, and a PaO2 of 92 mm Hg. Which intervention should the nurse implement?Reference Range:
Arterial Blood Gas (ABG)
pH [Adult/child: 7.35 to 7.45]
PaCO2 [Adult/child: 35 to 45 mm Hg)
HCO- [Adult/child: 21 to 28 mEq/L (21 to 28 mmol/L)] PaO2 [Adult/child: 80 to 100 mm Hg)
Increase rate of ventilation.
Decrease expiratory flow time.
Increase ventilator tidal volume.
Decrease expiratory pressure.
The Correct Answer is A
Rationale
A. The client's pH is low (acidotic), and the PaCO2 is high (respiratory acidosis). Increasing the rate of ventilation (respiratory rate) can help to decrease PaCO2 by increasing alveolar ventilation, thereby helping to correct respiratory acidosis.
B. Expiratory flow time affects the time available for exhalation. While this may affect the overall mechanics of ventilation, it is not directly targeting the primary issue of elevated PaCO2 and acidosis.
C. Increasing tidal volume increases the volume of air delivered with each breath. This can improve ventilation efficiency but may not address the underlying problem of elevated PaCO2 unless it leads to increased minute ventilation.
D. Expiratory pressure is related to positive end-expiratory pressure (PEEP), which helps maintain alveolar recruitment and improve oxygenation. Decreasing expiratory pressure may not directly address the elevated PaCO2 and acidosis.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Rationale
A. Osteoarthritis is characterized by the gradual destruction of joint cartilage. Cartilage serves as a cushion between the bones in a joint, and its deterioration leads to pain, stiffness, and reduced joint function. As the cartilage wears away, bones may rub directly against each other, causing further pain and damage.
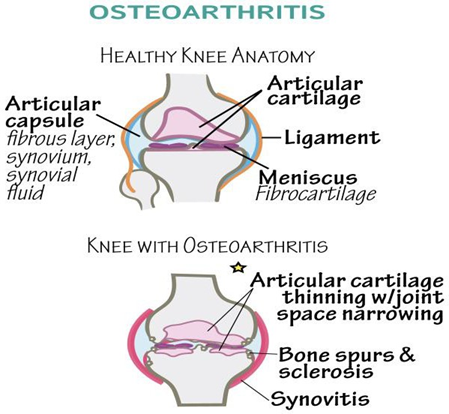
B. Osteoarthritis is primarily a degenerative condition rather than an inflammatory one. While mild inflammation can occur in OA, it is not as prominent as in autoimmune conditions like rheumatoid arthritis. In OA, inflammation is secondary to cartilage damage rather than a primary driver of the disease process.
C. Loss of bone mineral density is more characteristic of osteoporosis, a condition where bones become weak and brittle. Osteoporosis involves a decrease in bone mass throughout the skeleton, whereas osteoarthritis specifically targets the joints and affects cartilage rather than bone density.
D. An infectious process in the synovial fluid could indicate septic arthritis, which is characterized by infection in the joint space. This is typically associated with acute symptoms such as severe joint pain, swelling, warmth, and fever.
Correct Answer is B
Explanation
Rationale
A. Evacuation centers often accommodate a large number of people in close proximity. This can lead to increased transmission of infectious agents, including those causing diarrheal illnesses, through person- to-person contact or contaminated surfaces.
B. Hurricanes can cause flooding, which may overwhelm sewage systems and lead to contamination of drinking water sources. Consuming water contaminated by sewage can introduce pathogens that cause diarrheal diseases, such as bacteria like Escherichia coli or viruses like norovirus.
C. Flood waters can contaminate food supplies in various ways, such as direct contact with contaminated water, improper storage, or inadequate cooking or refrigeration. Consuming
contaminated food can result in diarrheal illnesses due to ingestion of pathogens like bacteria or parasites.
D. Nosocomial infections refer to infections acquired in healthcare settings. In a disaster medical area, improper infection control practices or overcrowding can contribute to nosocomial transmission of infectious agents, including those causing diarrheal diseases. However, this option is less likely in the context of a client seeking treatment for diarrhea immediately upon arrival at the disaster medical area.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
