Clinical Presentation of MDD
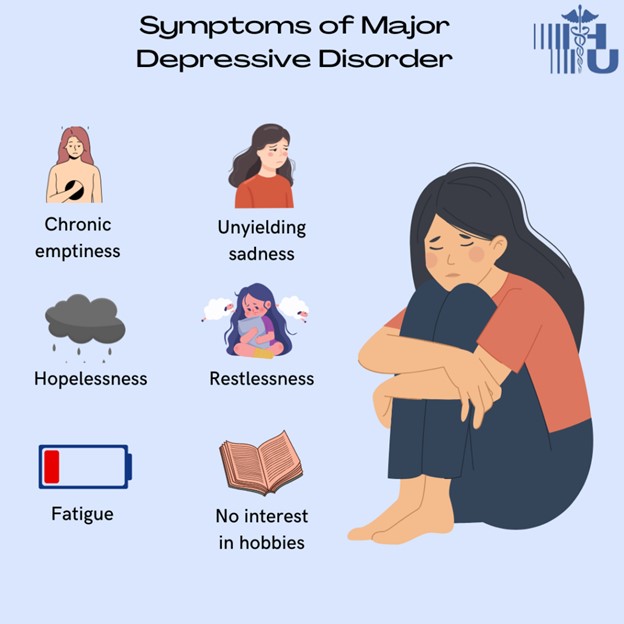
- The signs and symptoms of MDD vary from person to person but generally include:
- Depressed mood most of the day, nearly every day
- Markedly diminished interest or pleasure in all or almost all activities most of the day
- Significant weight loss or weight gain (more than 5% of body weight in a month) or appetite changes
- Insomnia or hypersomnia (excessive sleeping)
- Psychomotor agitation or retardation (observable by others)
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Diminished ability to think or concentrate or indecisiveness
- Recurrent thoughts of death or suicide or suicide attempts
- The diagnostic criteria for MDD according to DSM-5 are
- Five or more of the above symptoms must be present during the same 2-week period and represent a change from previous functioning
- At least one of the symptoms must be either depressed mood or loss of interest or pleasure
- The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
- The symptoms are not due to the direct effects of a substance or a medical condition
- The symptoms are not better explained by another mental disorder
- There has never been a manic episode or a hypomanic episode
- The assessment and screening tools for MDD include
- Patient Health Questionnaire (PHQ-9): a 9-item self-report questionnaire that measures the severity of depression based on the DSM-5 criteria. A score of 10 or higher indicates moderate to severe depression.
- Hamilton Depression Rating Scale (HAM-D): a 17-item clinician-administered scale that evaluates various aspects of depression such as mood, anxiety, insomnia, somatic symptoms, etc. A score of 20 or higher indicates severe depression.
- Beck Depression Inventory (BDI): a 21-item self-report inventory that assesses cognitive, affective, behavioral, and somatic symptoms of depression. A score of 30 or higher indicates severe depression.
- The differential diagnosis for MDD includes:
- Bipolar disorder: characterized by episodes of mania (elevated mood) or hypomania (mild mania) alternating with episodes of depression. A history of manic or hypomanic episodes rules out MDD.
- Dysthymia: a chronic form of depression that lasts for at least 2 years but is less severe than MDD. Dysthymia can coexist with MDD as a double depression.
- Adjustment disorder: a reaction to a stressful life event that causes emotional distress and impairment in functioning. Adjustment disorder usually resolves within 6 months after the stressor is removed or adapted to.
- Bereavement: a normal and expected response to the loss of a loved one that involves grief and sadness. Bereavement can be complicated by MDD if the symptoms are persistent, severe, or interfere with daily functioning.
- Substance-induced mood disorder: a mood disturbance that is caused by the use or withdrawal of a substance such as alcohol, drugs, or medications. The mood symptoms usually remit when the substance is discontinued or detoxified.
- Mood disorder due to a general medical condition: a mood disturbance that is caused by a physical illness or injury that affects the brain or other organs. The mood symptoms usually improve when the medical condition is treated.
Nursing Test Bank
Quiz #1: RN Exams Pharmacology Exams
Quiz #2: RN Exams Medical-Surgical Exams
Quiz #3: RN Exams Fundamentals Exams
Quiz #4: RN Exams Maternal-Newborn Exams
Quiz #5: RN Exams Anatomy and Physiology Exams
Quiz #6: RN Exams Obstetrics and Pediatrics Exams
Quiz #7: RN Exams Fluid and Electrolytes Exams
Quiz #8: RN Exams Community Health Exams
Quiz #9: RN Exams Promoting Health across the lifespan Exams
Quiz #10: RN Exams Multidimensional care Exams
Naxlex Comprehensive Predictor Exams
Quiz #1: Naxlex RN Comprehensive online practice 2019 B with NGN
Quiz #2: Naxlex RN Comprehensive Predictor 2023
Quiz #3: Naxlex RN Comprehensive Predictor 2023 Exit Exam A
Quiz #4: Naxlex HESI Exit LPN Exam
Quiz #5: Naxlex PN Comprehensive Predictor PN 2020
Quiz #6: Naxlex VATI PN Comprehensive Predictor 2020
Quiz #8: Naxlex PN Comprehensive Predictor 2023 - Exam 1
Quiz #10: Naxlex HESI PN Exit exam
Quiz #11: Naxlex HESI PN EXIT Exam 2
Questions on Clinical Presentation of MDD
Correct Answer is A
Explanation
<p> MDD cannot be diagnosed if only one symptom is present. The diagnosis requires the presence of multiple symptoms, including depressed mood or anhedonia, for at least two weeks.</p>
Correct Answer is ["C","D"]
Explanation
Elevated mood and increased energy are actually more indicative of conditions like bipolar disorder or manic episodes, where there are distinct periods of abnormally elevated mood, known as mania or hypomania.
Correct Answer is C
Explanation
Adjustment disorder is a condition characterized by emotional or behavioral symptoms that develop in response to a specific stressor. The client's statement is more indicative of a pervasive and ongoing lack of enjoyment, which aligns with the concept of anhedonia in MDD rather than the time-limited nature of adjustment disorder.
Correct Answer is D
Explanation
Criteria for diagnosing MDD according to DSM-5. The client's symptoms of extreme fatigue, difficulty concentrating, and thoughts of worthlessness align with the criteria for Major Depressive Disorder (MDD) as defined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). These criteria include the presence of specific symptoms for a specified duration, causing significant impairment in functioning. The symptoms should not be better explained by other conditions or substances. In this case, the client's presentation closely matches the criteria for diagnosing MDD.
Correct Answer is D
Explanation
"Dysthymia is chronic and lasts for at least 2 years, but is less severe than MDD." This statement is accurate. Dysthymia is a chronic form of depression that persists for at least two years. While it may not exhibit the same level of severity as a major depressive episode, its long-term nature can still have a substantial impact on an individual's quality of life. This distinguishes it from MDD, which can have episodic occurrences.
Correct Answer is A
Explanation
Mini-Mental State Examination (MMSE). The Mini-Mental State Examination (MMSE) is not an appropriate tool for assessing depression. Instead, it's a brief cognitive screening test used to assess cognitive impairment and cognitive decline in individuals, especially in older adults. It evaluates aspects such as orientation, memory, attention, language, and visuospatial skills. It is not designed to assess mood, anxiety, or other emotional aspects related to depression.
Correct Answer is C
Explanation
A normal response to stress usually involves transient feelings of sadness or anxiety in response to a stressor. However, the client's symptoms of persistent feelings of sadness, guilt, worthlessness, weight loss, and insomnia are indicative of a more serious and prolonged condition like major depressive disorder (MDD).
Correct Answer is ["A","C","E"]
Explanation
The correct answer. Chronic medical conditions are risk factors for developing major depressive disorder (MDD). The stress, emotional toll, and physiological effects of living with a chronic illness can contribute to the onset or exacerbation of depressive symptoms.
Correct Answer is ["C","E"]
Explanation
The correct answer. To meet the diagnostic criteria for major depressive disorder (MDD) according to DSM-5, an individual must experience five or more symptoms of depression during a continuous two-week period. These symptoms must include either depressed mood or loss of interest/pleasure. The scenario did not specify all the symptoms, but the persistent feelings of sadness, guilt, worthlessness, weight loss, and insomnia described align with the criteria.
Correct Answer is B
Explanation
<p>Adjustment disorder is characterized by the development of emotional or behavioral symptoms in response to an identifiable stressor, and these symptoms typically resolve within six months of the stressor's resolution. In the scenario, there is no indication of a recent stressor, and the client's symptoms seem to be chronic rather than time-limited, making adjustment disorder less likely.</p>
Environmental theory suggests that external factors, such as life events and stressors, contribute to the development of depression. While environment can indeed influence depression, it does not specifically address the neurotransmitter imbalances that are central to this question.
Interpersonal relationships are affected by depression and can also contribute to its development. The question does not focus on the effects of depression on relationships, but rather on the factors that can influence or be influenced by depression.
This statement is not accurate. Chronic stress tends to lead to hyperactivity of the HPA axis and elevated cortisol levels. Reduced cortisol levels, as suggested in this choice, are not commonly associated with chronic stress and its impact on depression.
Cognitive-behavioral therapy (CBT) is a specific type of psychotherapeutic intervention that focuses on changing thought patterns and behaviors. While CBT can lead to changes in brain activity and neuroplasticity, it does not involve direct brain stimulation through electrical or magnetic means like
Excessive energy is not a common side effect associated with antidepressant use. Antidepressants typically work to regulate mood and alleviate symptoms of depression, and excessive energy would not align with the expected effects of these medications.
Endorphins and oxytocin are important neurotransmitters, but they are not as directly related to the regulation of mood, motivation, reward, cognition, and stress response as the neurotransmitters mentioned in choice C. Endorphins are known for their role in pain modulation and feelings of pleasure,
Optimistic thinking is typically considered a protective factor against depression rather than a contributor to its development. Optimistic thinking involves a positive outlook on life and the expectation of positive outcomes, which can act as a resilience factor against depressive symptoms.
Neurotransmitter imbalances are not psychosocial factors. They are more related to the biological underpinnings of depression rather than the social and psychological influences explored in psychosocial factors.
Mindfulness-based cognitive therapy (MBCT) is a psychological approach that combines mindfulness meditation with cognitive behavioral techniques. While MBCT has shown promise in preventing relapse for individuals with recurrent depression, it's usually used as a psychotherapeutic adjunct to other ma
This is the correct answer. Genetic factors do contribute to an individual's vulnerability to depression. Studies of families, twins, and heritability have demonstrated a genetic component to depression. However, it's crucial to recognize that genetic predisposition interacts with environmental fact
Search Here
Related Topics
- Types of Eating Disorders DSM 5 - Mood Disorders and Suicide
- Obsessive-compulsive disorders - Mood Disorders and Suicide
- Clinical Picture of Abuse and Violence - Mood Disorders and Suicide
- Child and Elder Abuse - Mood Disorders and Suicide
- Child Abuse - Mood Disorders and Suicide
- Elder Abuse - Mood Disorders and Suicide
More on Nursing
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
