Which term would the nurse use when extracellular fluid and intracellular fluid have the same osmolality?
Hypotonic
Oncotic pressure
Isotonic
Hypertonic
The Correct Answer is C
Choice A: Hypotonic
A hypotonic solution has a lower concentration of solutes compared to the fluid inside the cells. When cells are placed in a hypotonic solution, water enters the cells, causing them to swell and potentially burst. This is because the osmotic pressure drives water into the cells to balance the solute concentration. Hypotonic solutions are not used to describe a state where extracellular and intracellular fluids have the same osmolality.
Choice B: Oncotic Pressure
Oncotic pressure, also known as colloid osmotic pressure, is the form of osmotic pressure exerted by proteins, primarily albumin, in the blood plasma. It plays a crucial role in maintaining fluid balance between the blood vessels and the surrounding tissues by pulling water into the circulatory system. Oncotic pressure is not related to the concept of equal osmolality between extracellular and intracellular fluids.
Choice C: Isotonic
An isotonic solution has the same concentration of solutes as the fluid inside the cells. When extracellular fluid is isotonic to intracellular fluid, there is no net movement of water into or out of the cells, maintaining cell stability. This balance is crucial for normal cellular function and is the term used to describe equal osmolality between extracellular and intracellular fluids.
Choice D: Hypertonic
A hypertonic solution has a higher concentration of solutes compared to the fluid inside the cells. When cells are placed in a hypertonic solution, water leaves the cells, causing them to shrink or crenate. This occurs because the osmotic pressure drives water out of the cells to balance the solute concentration. Hypertonic solutions are not used to describe a state where extracellular and intracellular fluids have the same osmolality.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A: Show the caregiver how to check the patient’s temperature and blood pressure
Showing the caregiver how to check the patient’s temperature and blood pressure involves direct patient education and demonstration, which requires the clinical judgment and expertise of a licensed nurse. This task ensures that the caregiver understands the correct techniques and can accurately monitor the patient’s vital signs. Delegating this task to assistive personnel (AP) is not appropriate because it requires a higher level of skill and knowledge to teach and verify understanding.
Choice B: Give the patient a pamphlet that reinforces teaching done by the nurse
Giving the patient a pamphlet that reinforces teaching done by the nurse is a task that can be delegated to assistive personnel (AP). This action does not require clinical judgment or advanced skills. The pamphlet serves as a supplementary resource to the verbal and hands-on education provided by the nurse. It is a straightforward task that AP can perform, ensuring that the patient has access to written information that reinforces the nurse’s teaching.
Choice C: Evaluate whether the patient and caregiver understand the teaching
Evaluating whether the patient and caregiver understand the teaching is a critical component of the discharge process that requires the clinical judgment of a licensed nurse. This task involves assessing the patient’s and caregiver’s comprehension, identifying any gaps in understanding, and providing additional education as needed. It is not appropriate to delegate this responsibility to assistive personnel (AP) because it requires professional assessment skills.
Choice D: Plan topics for the discharge teaching session with the patient and caregiver
Planning topics for the discharge teaching session with the patient and caregiver involves developing a comprehensive and individualized teaching plan based on the patient’s specific needs and condition. This task requires the expertise and clinical judgment of a licensed nurse to ensure that all relevant topics are covered and that the teaching plan is tailored to the patient’s situation. Delegating this task to assistive personnel (AP) is not appropriate because it requires advanced planning and professional knowledge.
Correct Answer is C
Explanation
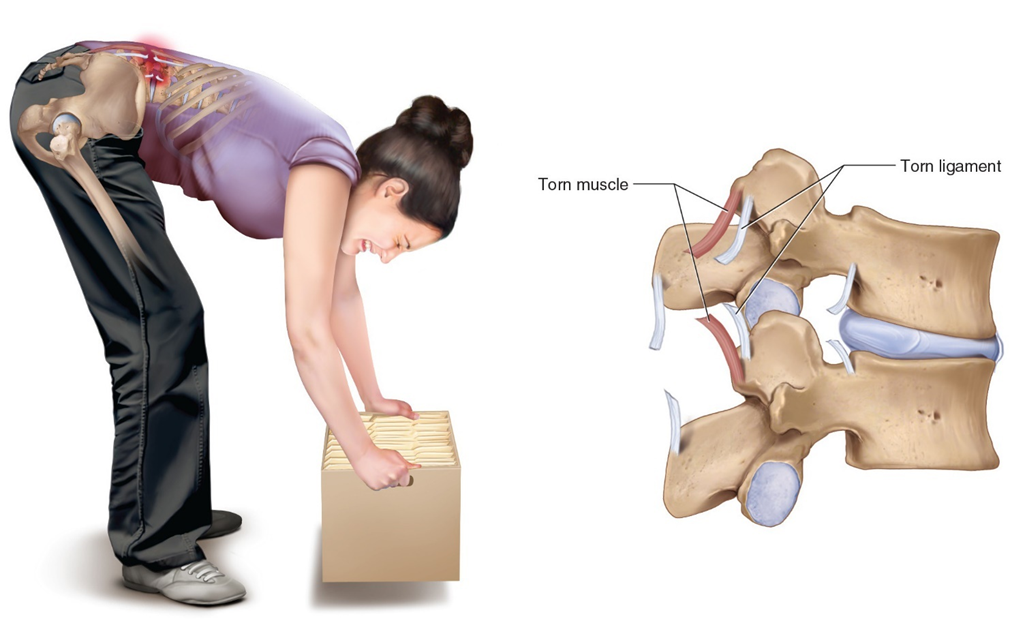
Choice A: Promote healing by increasing the rate of the muscle remodeling process
While heat can aid in the healing process by improving blood flow and nutrient delivery to the injured area, it does not specifically increase the rate of the muscle remodeling process. Muscle remodeling involves complex cellular activities that are not solely influenced by external heat application.
Choice B: Decrease pain by reducing inflammation
Heat therapy is generally not used to reduce inflammation. In fact, applying heat to an inflamed area can sometimes exacerbate the inflammation. Cold therapy is more effective for reducing inflammation, especially in the initial stages of an injury.
Choice C: Decrease pain by increasing circulation to a painful area and relaxing tense muscles
This is the correct answer. Applying heat to a painful area causes vasodilation, which increases blood flow and helps deliver oxygen and nutrients to the affected tissues. This process helps to relax tense muscles and alleviate pain. Heat therapy is particularly effective for muscle spasms, stiffness, and chronic pain conditions.
Choice D: Decrease pain by numbing pain signals
Heat therapy does not numb pain signals in the same way that cold therapy does. Cold therapy works by numbing the affected area and reducing nerve activity, which helps to alleviate pain. Heat therapy, on the other hand, works by improving circulation and relaxing muscles.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
