The following 4 questions pertain to this case study:
Which task is appropriate for the nurse to delegate to experienced certified nurse assistant (CNA)?
Monitor for shortness of breath or fatigue after ambulation.
Determine whether the patient is ready to increase activity.
Obtain the patient’s blood pressure and pulse rate after ambulation.
Instruct the patient on how to use an incentive spirometer.
The Correct Answer is C
Choice A reason:
Monitoring for shortness of breath or fatigue after ambulation is a critical task that requires clinical judgment and assessment skills. Certified Nurse Assistants (CNAs) are trained to assist with basic patient care activities but are not typically trained to assess and interpret clinical symptoms such as shortness of breath or fatigue. These symptoms could indicate serious complications such as pulmonary embolism or cardiac issues, which require immediate attention from a licensed nurse or physician. Therefore, this task is not appropriate for delegation to a CNA.
Choice B reason:
Determining whether the patient is ready to increase activity involves assessing the patient’s overall condition, including their vital signs, pain levels, and physical capabilities. This requires a comprehensive understanding of the patient’s medical history and current status, which falls within the scope of practice of a registered nurse (RN) or licensed practical nurse (LPN). CNAs do not have the training to make such determinations, as it involves critical thinking and clinical decision-making skills. Therefore, this task should not be delegated to a CNA.
Choice C reason:
Obtaining the patient’s blood pressure and pulse rate after ambulation is a task that is appropriate for delegation to a CNA. CNAs are trained to measure and record vital signs, including blood pressure and pulse rate. This task does not require clinical judgment or decision-making, making it suitable for delegation. The CNA can report the findings to the nurse, who can then interpret the results and make any necessary clinical decisions. This delegation allows the nurse to focus on more complex tasks that require their advanced training and expertise.
Choice D reason:
Instructing the patient on how to use an incentive spirometer involves patient education, which is a responsibility that typically falls to licensed nurses. Proper use of an incentive spirometer is crucial for preventing postoperative complications such as atelectasis and pneumonia. Ensuring that the patient understands how to use the device correctly requires not only demonstrating its use but also assessing the patient’s comprehension and ability to perform the task. This level of patient education and assessment is beyond the scope of practice for a CNA.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A: 3% Saline
3% Saline is a hypertonic solution, meaning it has a higher concentration of solutes compared to the blood plasma. It is typically used in critical care settings for specific conditions such as severe hyponatremia or cerebral edema. Administering 3% Saline to a patient with a fluid deficit who requires isotonic fluid replacement would not be appropriate because it could lead to cellular dehydration and other complications due to its high osmolarity.
Choice B: Saline 0.45%
Saline 0.45%, also known as half-normal saline, is a hypotonic solution. It has a lower concentration of solutes compared to blood plasma and is used to treat patients with hypernatremia or those who need to be rehydrated without adding too much sodium. However, it is not suitable for isotonic fluid replacement because it can cause cells to swell and potentially burst due to the influx of water into the cells.
Choice C: Saline 0.9%
Saline 0.9%, also known as normal saline, is an isotonic solution. It has the same concentration of solutes as blood plasma, making it ideal for fluid replacement in patients with a fluid deficit. Normal saline is commonly used to expand the extracellular fluid volume without causing significant shifts in fluid between compartments. This makes it the appropriate choice for isotonic fluid replacement.
Choice D: Dextrose 10%
Dextrose 10% is a hypertonic solution used primarily for providing calories in patients who need parenteral nutrition or for treating severe hypoglycemia. It is not suitable for isotonic fluid replacement because its high glucose content can lead to osmotic diuresis and fluid shifts that are not desirable in patients needing isotonic fluids.
Correct Answer is A
Explanation
Choice A: Infuse the KCl at a maximum rate of 10 mEq/hr
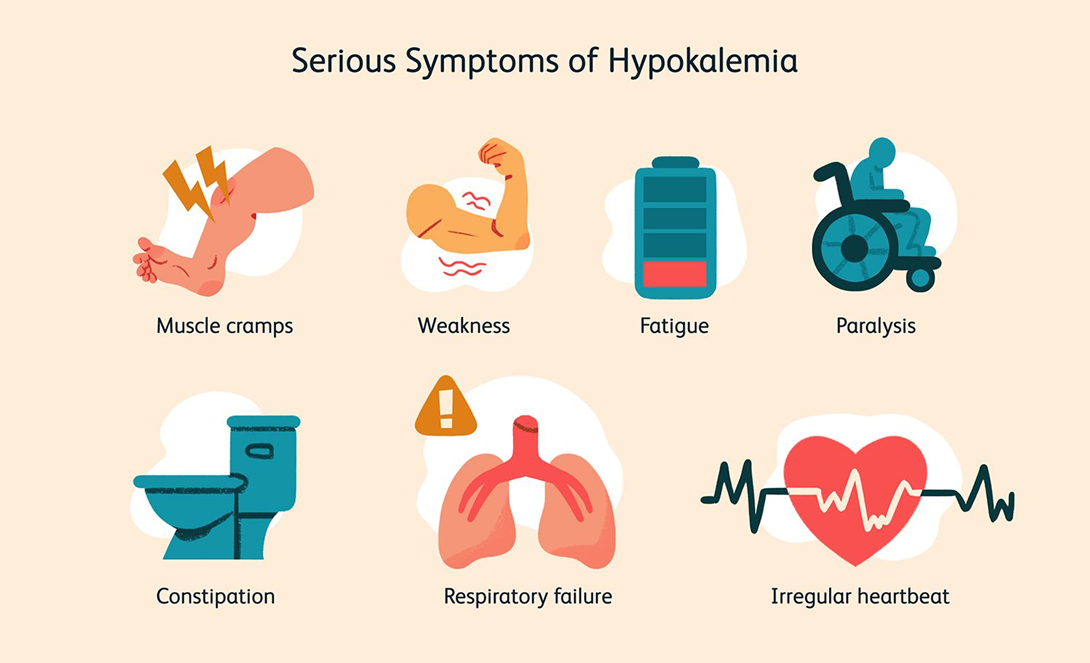
This is the correct answer. The recommended infusion rate for potassium chloride is generally not to exceed 10 mEq per hour to avoid complications such as hyperkalemia and cardiac arrhythmias. This rate ensures that the potassium is administered safely and effectively, allowing for proper monitoring and adjustment if necessary.
Choice B: Discontinue cardiac monitoring during the infusion
This choice is incorrect. Cardiac monitoring is essential during the infusion of potassium chloride, especially in patients with severe hypokalemia, due to the risk of arrhythmias and other cardiac complications. Continuous monitoring allows for the early detection of any adverse effects and timely intervention.
Choice C: Administer the KCl as a rapid IV bolus
Administering potassium chloride as a rapid IV bolus is dangerous and contraindicated. Rapid infusion can lead to severe hyperkalemia, which can cause fatal cardiac arrhythmias. Potassium chloride should always be administered slowly and diluted in an appropriate volume of fluid.
Choice D: Refuse to give the KCl through a peripheral venous line
While central lines are preferred for higher concentrations of potassium chloride due to the risk of irritation and phlebitis, peripheral lines can be used for lower concentrations and slower infusion rates. Refusing to administer potassium chloride through a peripheral line is not necessary if the infusion is properly managed and monitored.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
