Which six factors should the nurse consider when choosing a time frame for reassessing the patient’s pain level after implementing pain management?
Agency policy
Type of intervention
Pain severity
If family members are present in the patient’s room
The patient’s psychosocial condition
Risks for adverse effects
Workload of the nurse
The patient’s physical condition
Correct Answer : B,C,E,F,H
Choice A: Agency policy
While agency policy provides guidelines for reassessment intervals, it is not the primary factor in determining the specific time frame for reassessing a patient’s pain level. Policies serve as a general framework, but individual patient needs and clinical judgment should guide the reassessment timing.
Choice B: Type of intervention
This is a correct answer. The type of pain management intervention used significantly influences the reassessment time frame. For example, after administering intravenous pain medication, reassessment should occur sooner compared to oral medications due to the faster onset of action. Different interventions have varying durations of effectiveness, necessitating tailored reassessment intervals.
Choice C: Pain severity
This is another correct answer. The severity of the patient’s pain is a crucial factor in determining reassessment timing. Patients experiencing severe pain may require more frequent reassessments to ensure that pain management strategies are effective and to make timely adjustments if needed.
Choice D: If family members are present in the patient’s room
The presence of family members in the patient’s room is not a primary factor in determining the reassessment time frame. While family members can provide valuable support and information, the focus should remain on the patient’s clinical needs and the effectiveness of pain management interventions.
Choice E: The patient’s psychosocial condition
This is a correct answer. The patient’s psychosocial condition, including their emotional and mental state, can impact their perception of pain and response to pain management. Patients with anxiety, depression, or other psychosocial issues may require more frequent reassessments to address both physical and emotional aspects of pain.
Choice F: Risks for adverse effects
This is also a correct answer. The potential for adverse effects from pain management interventions necessitates careful monitoring and timely reassessment. For instance, opioids carry risks of respiratory depression and sedation, requiring close observation and frequent reassessment to ensure patient safety.
Choice G: Workload of the nurse
While the nurse’s workload can influence the practical aspects of care delivery, it should not dictate the reassessment time frame. Patient needs and clinical priorities should guide reassessment intervals, with workload management being a secondary consideration.
Choice H: The patient’s physical condition
This is the final correct answer. The patient’s overall physical condition, including comorbidities and current health status, affects their response to pain management and the need for reassessment. Patients with complex medical conditions may require more frequent monitoring to ensure effective pain control and to promptly address any complications.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A: Alkalosis
Alkalosis occurs when the blood pH is higher than the normal range, specifically above 7.45. This condition indicates that the blood is too alkaline. Causes of alkalosis can include hyperventilation, loss of stomach acid through vomiting, or an overuse of diuretics. Since a blood pH of 7.21 is below the normal range, it does not indicate alkalosis.
Choice B: Normal Blood pH
The normal pH range for blood is between 7.35 and 7.45. This range is crucial for the body’s metabolic processes and enzyme functions. A blood pH of 7.21 is below this range, indicating an abnormal condition.
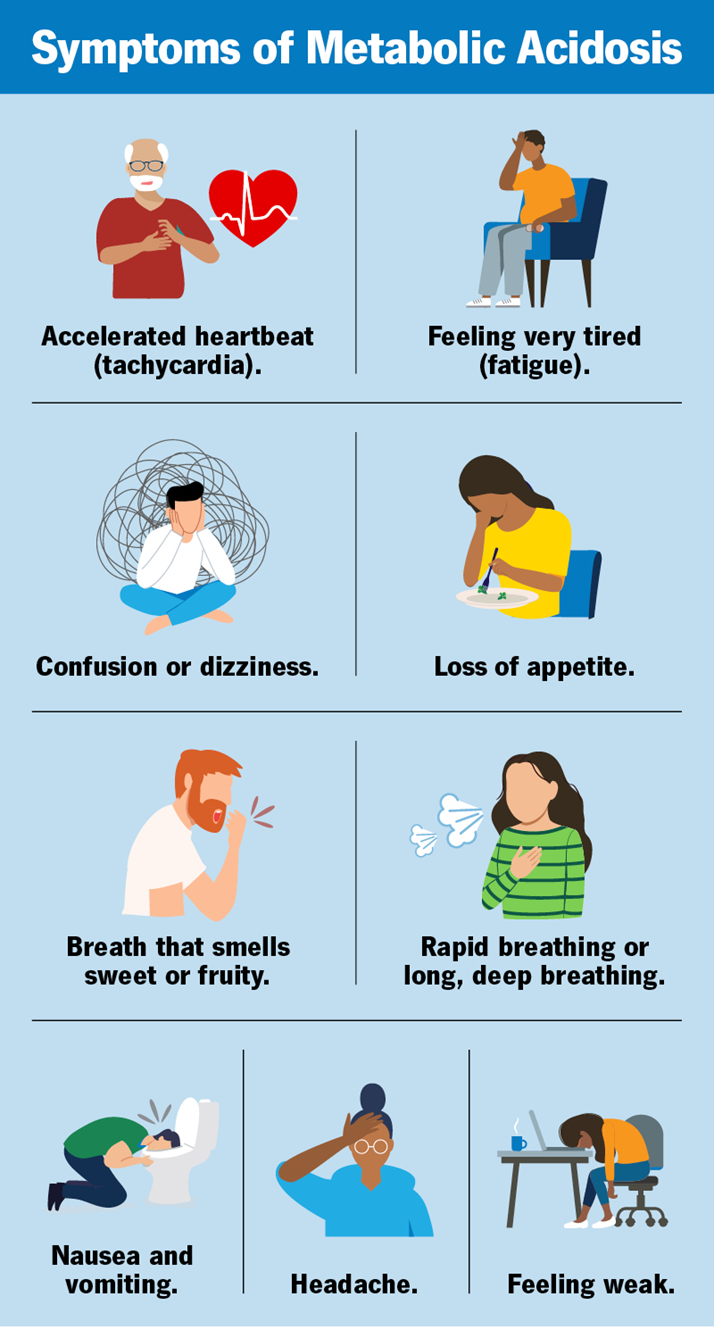
Choice C: Acidosis
Acidosis is the correct answer. It occurs when the blood pH drops below 7.35, indicating that the blood is too acidic. A pH of 7.21 is significantly below the normal range, confirming acidosis. This condition can result from various factors, including respiratory issues that lead to an accumulation of carbon dioxide or metabolic problems that increase acid production or decrease bicarbonate levels.
Choice D: Hyperkalemia
Hyperkalemia refers to an elevated level of potassium in the blood, not a change in blood pH. While hyperkalemia can be associated with acidosis, it is not defined by the pH level itself. Therefore, a blood pH of 7.21 does not directly indicate hyperkalemia.
Correct Answer is ["A","C","D","E"]
Explanation
Choice A reason:
Notifying the oncologist or healthcare provider immediately is crucial in the event of a reaction or side effect during chemotherapy. Prompt communication with the healthcare provider ensures that the patient receives appropriate and timely medical intervention. The oncologist can provide specific instructions on managing the reaction, including any necessary medications or adjustments to the chemotherapy regimen. Immediate notification helps in preventing the escalation of the reaction and ensures patient safety.
Choice B reason:
Slowing the chemotherapy infusion is not typically recommended as an immediate intervention for a severe reaction. While adjusting the infusion rate can be considered for mild reactions, it is not sufficient for managing more serious side effects or hypersensitivity reactions. In cases of significant reactions, stopping the infusion and taking other emergency measures are more appropriate. Slowing the infusion might delay the necessary interventions and could potentially worsen the patient’s condition.
Choice C reason:
Stopping the chemotherapy infusion is a critical step in managing a reaction. Halting the infusion immediately prevents further exposure to the causative agent, which can help in stabilizing the patient’s condition. This action is essential to prevent the reaction from worsening and allows time for the healthcare team to assess the situation and implement appropriate interventions. Stopping the infusion is a standard protocol in managing infusion-related reactions.
Choice D reason:
Assessing Ms. Anderson’s vital signs and symptoms is essential to determine the severity of the reaction and guide further interventions. Monitoring vital signs such as heart rate, blood pressure, respiratory rate, and oxygen saturation provides crucial information about the patient’s physiological status. This assessment helps in identifying any life-threatening changes and ensures that appropriate measures are taken to stabilize the patient. Continuous monitoring is vital for detecting any deterioration in the patient’s condition.
Choice E reason:
Infusing normal saline at 100 ml/hr is an important intervention to maintain intravenous access and provide fluid support. Normal saline helps in stabilizing the patient’s blood pressure and improving circulation, which can be compromised during a severe reaction. It also ensures that the IV line remains patent for the administration of emergency medications if needed. Fluid support is a key component of managing infusion-related reactions and preventing complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
