What is the main function of the Na-K pump at the cellular level?
Move Na inside the cell
Move K out of the cell
Move Na out of the cell
Move Na and K inside the cell
The Correct Answer is C
Choice A: Move Na Inside the Cell
The primary function of the Na-K pump, also known as the sodium-potassium pump, is to move sodium (Na) ions out of the cell, not into the cell. This pump actively transports three sodium ions out of the cell for every two potassium ions it brings in. Therefore, this choice is incorrect.
Choice B: Move K Out of the Cell
The Na-K pump moves potassium (K) ions into the cell, not out of the cell. This active transport mechanism helps maintain the necessary concentration gradients of sodium and potassium across the cell membrane, which are crucial for various cellular functions, including maintaining the resting membrane potential.
Choice C: Move Na Out of the Cell
The main function of the Na-K pump is to move sodium ions out of the cell. For every cycle of the pump, three sodium ions are exported out of the cell, and two potassium ions are imported into the cell. This process is essential for maintaining the electrochemical gradient across the cell membrane, which is vital for nerve impulse transmission, muscle contraction, and overall cellular homeostasis.
Choice D: Move Na and K Inside the Cell
This choice is incorrect because the Na-K pump does not move both sodium and potassium ions inside the cell. Instead, it moves sodium ions out of the cell and potassium ions into the cell. This active transport mechanism is crucial for maintaining the proper ionic balance and membrane potential necessary for various physiological processes.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
Norepinephrine is a key neurotransmitter released by the sympathetic nervous system during the “fight-or-flight” response. It plays a crucial role in preparing the body to respond to stress by increasing heart rate, blood pressure, and blood flow to muscles, as well as dilating the airways. These physiological changes are essential for coping with acute stress.
Choice B Reason:
Cortisol is a hormone released by the adrenal glands in response to stress, but it is primarily associated with the hypothalamic-pituitary-adrenal (HPA) axis rather than the sympathetic nervous system. While cortisol contributes to the body’s overall stress response by increasing blood sugar levels and suppressing the immune system, it is not the primary mediator of the acute “fight-or-flight” response.
Choice C Reason:
ACTH (adrenocorticotropic hormone) is a hormone produced by the pituitary gland that stimulates the adrenal glands to release cortisol. It is part of the HPA axis and plays a role in the body’s long-term stress response, but it is not directly involved in the immediate activation of the sympathetic nervous system.
Choice D Reason:
Glucagon is a hormone produced by the pancreas that raises blood glucose levels by promoting the breakdown of glycogen to glucose in the liver. While it can be involved in the body’s response to stress by ensuring an adequate supply of glucose, it is not a primary mediator of the acute stress response mediated by the sympathetic nervous system.
Correct Answer is A
Explanation
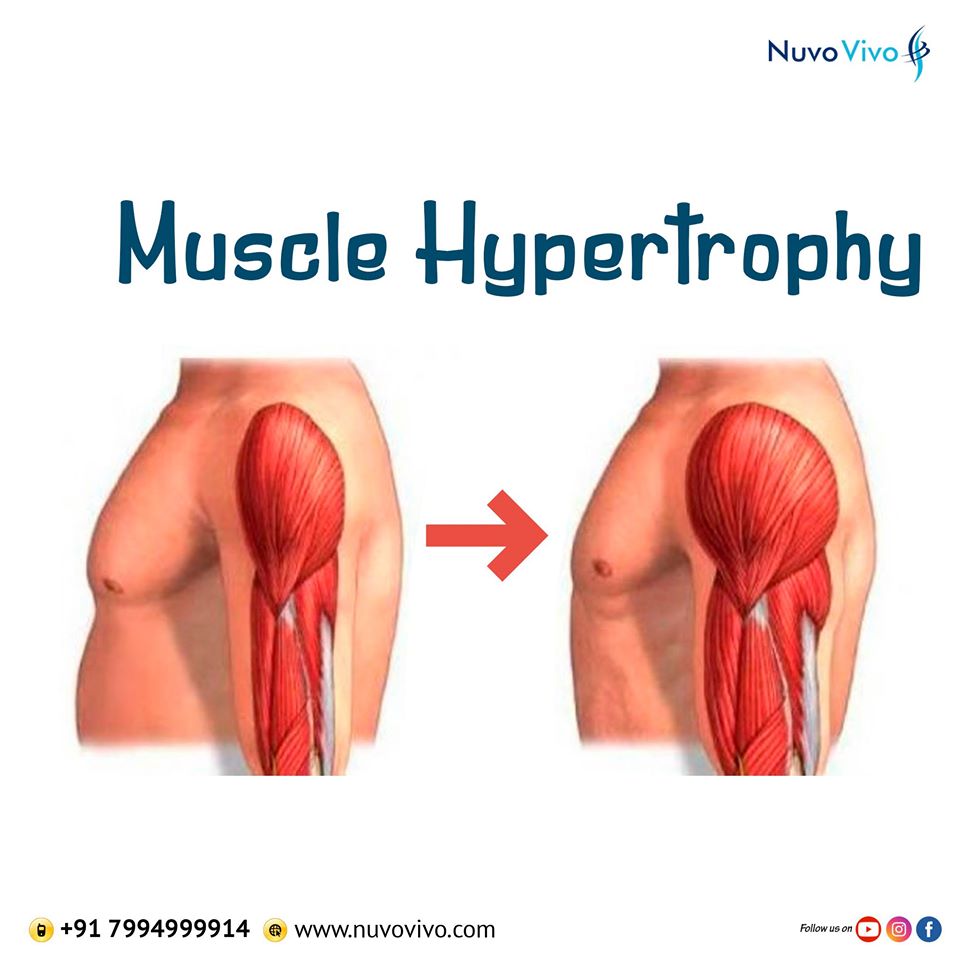
Choice A: Size
Muscular hypertrophy refers to the increase in the size of muscle cells12. This process typically occurs as a result of strength training, where the muscles are subjected to stress and damage, leading to the repair and growth of muscle fibers. The increase in muscle cell size enhances muscle strength and mass, making it a key goal for athletes and bodybuilders.
Choice B: Vacuoles
Vacuoles are membrane-bound organelles found in cells, primarily involved in storage and transport of substances3. While vacuoles play important roles in cellular function, they are not directly related to muscular hypertrophy. The primary change in muscular hypertrophy is the increase in muscle cell size, not the number or size of vacuoles.
Choice C: Types
Muscle cells can be categorized into different types, such as slow-twitch (Type I) and fast-twitch (Type II) fibers4. However, muscular hypertrophy does not involve a change in the types of muscle cells. Instead, it focuses on the growth and enlargement of existing muscle fibers, regardless of their type.
Choice D: Number
An increase in the number of muscle cells is referred to as hyperplasia, which is different from hypertrophy. Hyperplasia involves the formation of new muscle cells, whereas hypertrophy involves the enlargement of existing muscle cells. Current evidence suggests that hypertrophy, rather than hyperplasia, is the primary mechanism for muscle growth in response to strength training.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
