The RN is aware that a long-term side effect of amiodarone is:
Stevens-Johnsons Syndrome.
Ventricular Tachycardia.
Pulmonary fibrosis.
QT Prolongation.
The Correct Answer is D
Choice A rationale:
Stevens-Johnson syndrome (SJS) is a rare, serious skin condition that is typically caused by an allergic reaction to medication. While amiodarone has been associated with a few cases of SJS, it is not considered a common long-term side effect.
Choice B rationale:
Ventricular tachycardia (VT) is a type of fast heart rhythm that originates in the ventricles of the heart. Amiodarone is actually used to treat VT, so it would be counterintuitive to list it as a long-term side effect.
Choice C rationale:
Pulmonary fibrosis is a condition characterized by scarring of the lung tissue. While amiodarone can cause pulmonary toxicity, which includes pulmonary fibrosis, this is a relatively rare side effect. Moreover, it's usually associated with high doses or
long-term use of the medication.
Choice D rationale:
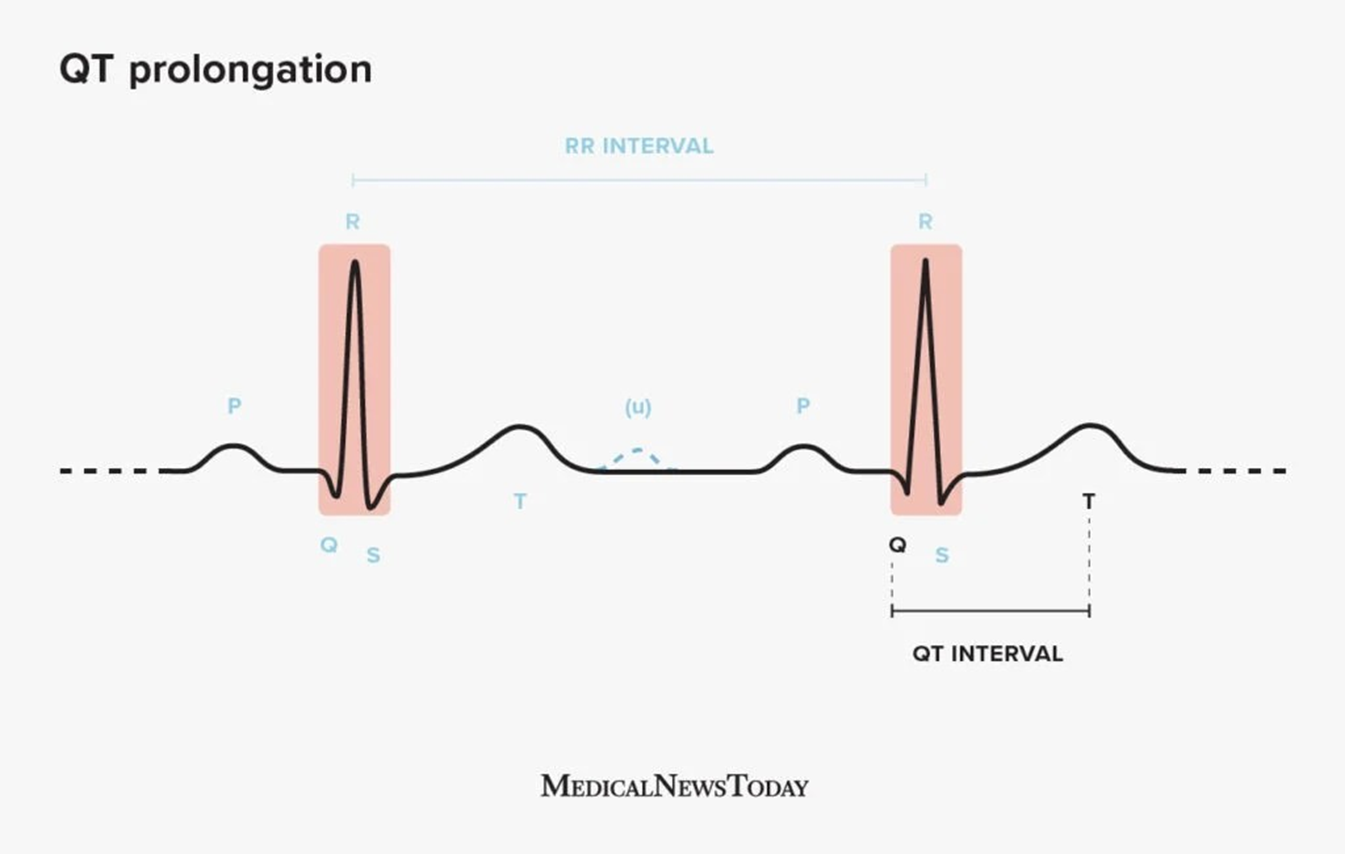
QT prolongation is a condition in which the heart's electrical activity takes longer than normal to recharge between beats. This can lead to a potentially fatal arrhythmia called torsades de pointes. Amiodarone is known to prolong the QT interval, and this is considered one of its most significant long-term side effects. It's important to monitor patients on amiodarone for QT prolongation and to adjust the dose or discontinue the medication if necessary.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["A","B","D"]
Explanation
Choice A rationale:
Seizure precautions are necessary because:
The patient has ingested multiple drugs, some of which can lower the seizure threshold, such as benzodiazepines. Naloxone, while reversing opioid overdose, can also precipitate seizures in some individuals.
Flumazenil, used to reverse benzodiazepine overdose, can also induce seizures, especially in patients with a history of epilepsy or benzodiazepine dependence.
The potential for drug interactions and unpredictable effects of multiple drug ingestion further increases the risk of seizures. Specific seizure precautions include:
Placing the patient in a bed with padded side rails. Having oxygen and suction equipment readily available.
Keeping intravenous access open for potential administration of anticonvulsant medications. Closely monitoring the patient's neurological status for any signs of seizure activity.
Choice B rationale:
Aspiration precautions are crucial due to:
The patient's unconscious state, which impairs their ability to protect their airway.
The possibility of vomiting, which can occur as a side effect of naloxone or flumazenil administration.
The potential for aspiration of gastric contents, which can lead to serious respiratory complications, such as pneumonia. Specific aspiration precautions include:
Positioning the patient on their side in the recovery position. Continuously monitoring the patient's respiratory status.
Having suction equipment ready to clear the airway if necessary.
Considering intubation and mechanical ventilation if the patient's airway is compromised.
Choice D rationale:
Fall precautions are essential because:
The patient is unconscious and may be disoriented or uncoordinated upon regaining consciousness.
The effects of the ingested drugs, as well as the medications administered, can impair balance and coordination. Falls can result in serious injuries, such as head trauma or fractures.
Specific fall precautions include:
Keeping the bed in a low position with side rails up.
Assisting the patient with ambulation when they are able to move. Ensuring the patient's environment is free of tripping hazards.
Providing close supervision and assistance as needed.
Choice C rationale:
Suicide precautions are not routinely implemented in this scenario because:
The patient's primary presentation is drug overdose, not active suicidal ideation or attempts.
The focus of care is on addressing the immediate medical complications of the overdose and stabilization.
However, a thorough suicide risk assessment should be conducted once the patient is medically stable to determine if ongoing suicide precautions are necessary.
Correct Answer is B
Explanation
Choice A rationale:
Digoxin is a cardiac glycoside, not a calcium channel blocker. It works by increasing the force of contraction of the heart muscle and slowing the heart rate. However, it is not typically used as a first-line treatment for tachycardia. It's more commonly used to treat heart failure and atrial fibrillation.
Mechanism of action: Digoxin inhibits the sodium-potassium ATPase pump in cardiac cells, leading to an increase in intracellular calcium. This increased calcium availability enhances myocardial contractility. Digoxin also indirectly affects the autonomic nervous system, leading to a decrease in heart rate.
Key points:
Digoxin is not a calcium channel blocker.
It's used primarily for heart failure and atrial fibrillation.
Its mechanism of action involves increasing intracellular calcium and decreasing heart rate.
Choice B rationale:
Diltiazem (Cardizem) is a calcium channel blocker that is commonly used to treat tachycardia and manage heart rate. It works by blocking the movement of calcium into cardiac cells, which slows down the electrical conduction system of the heart and leads to a decrease in heart rate.
Mechanism of action: Diltiazem blocks L-type calcium channels in cardiac and vascular smooth muscle cells. This reduces calcium influx, leading to:
Decreased myocardial contractility Vasodilation (relaxation of blood vessels)
Negative chronotropic effect (decreased heart rate)
Negative dromotropic effect (slowed conduction through the AV node) Key points:
Diltiazem is a calcium channel blocker.
It's effective in treating tachycardia and managing heart rate.
Its mechanism of action involves blocking calcium channels, leading to various cardiovascular effects.
Choice C rationale:
Nitroglycerin is a vasodilator, not a calcium channel blocker. It works by relaxing the smooth muscle in blood vessels, which widens the vessels and allows more blood to flow through them. This can help to relieve chest pain (angina) and lower blood pressure, but it does not directly affect heart rate.
Mechanism of action: Nitroglycerin is metabolized to nitric oxide, which activates guanylate cyclase, leading to increased production of cyclic guanosine monophosphate (cGMP). cGMP causes smooth muscle relaxation, resulting in vasodilation.
Key points:
Nitroglycerin is a vasodilator, not a calcium channel blocker. It's primarily used for angina and hypertension.
Its mechanism of action involves nitric oxide-mediated vasodilation.
Choice D rationale:
Nitroprusside (Nipride) is a potent vasodilator, not a calcium channel blocker. It is typically used in critical care settings to manage severe hypertension or heart failure. It works by relaxing the smooth muscle in blood vessels, which widens the vessels and allows more blood to flow through them. This can help to lower blood pressure, but it does not directly affect heart rate.
Mechanism of action: Nitroprusside directly releases nitric oxide, leading to vasodilation. Key points:
Nitroprusside is a potent vasodilator, not a calcium channel blocker.
It's used in critical care settings for severe hypertension or heart failure.
Its mechanism of action involves direct nitric oxide release and vasodilation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
