The RN in the intensive care unit has been administering ondansetron (Zofran) to a patient every 4-6 hours for nausea.
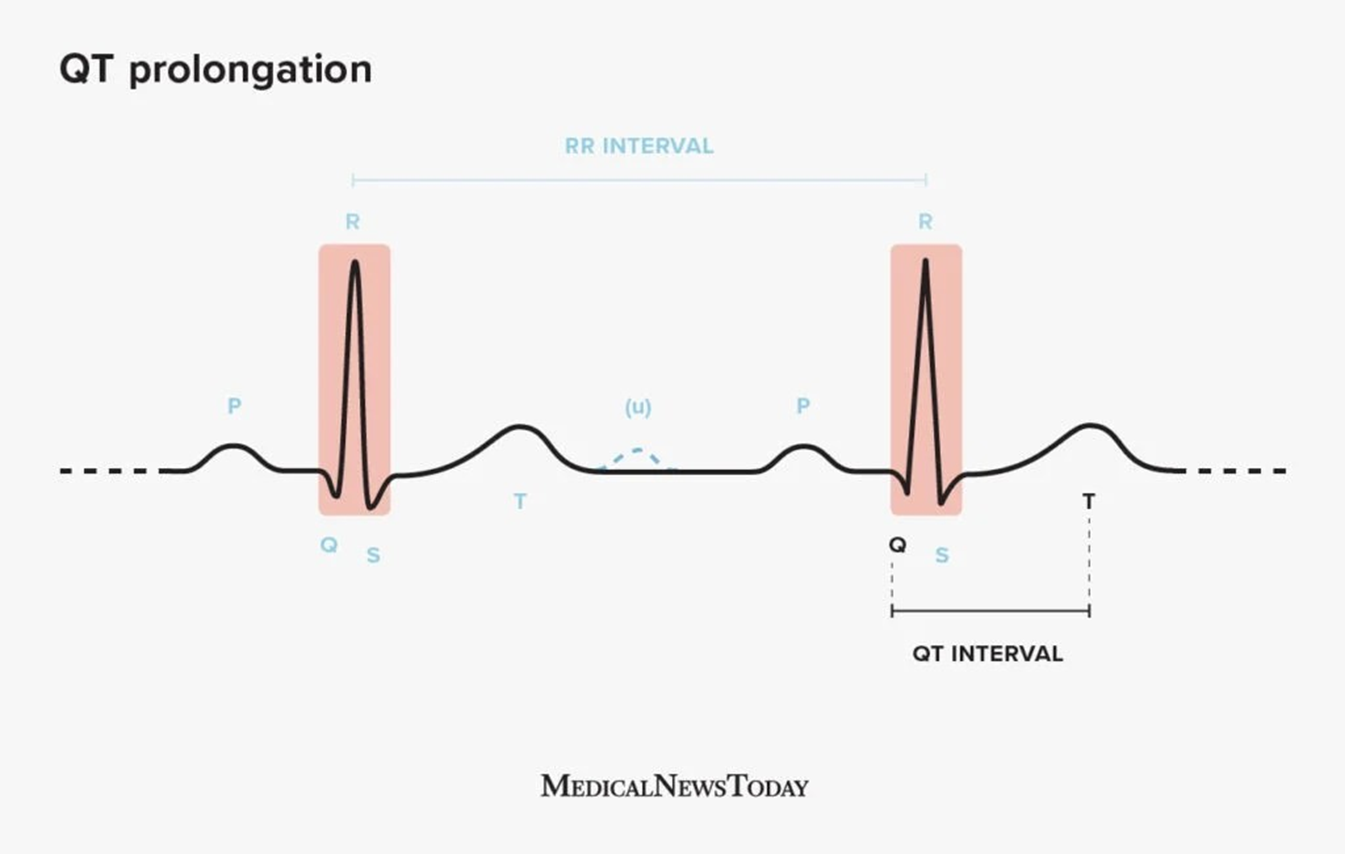
The RN notices that the patient has developed Q-T prolongation per the cardiac monitor.
Suddenly, the patient develops a wide-complex arrhythmia and is quickly determined to be in Torsades de Pointes. What is the 1st line drug for treatment?
Amiodarone.
Lidocaine.
Atropine.
Magnesium Sulfate.
The Correct Answer is D
Choice A rationale:
Amiodarone is an antiarrhythmic medication that is often used to treat ventricular tachycardia and ventricular fibrillation. However, it is not the first-line drug for Torsades de Pointes. In fact, amiodarone can actually worsen QT prolongation and increase the risk of Torsades de Pointes.
It's important to note that amiodarone has a long half-life and can accumulate in the body over time, further increasing the risk of QT prolongation.
Additionally, amiodarone can have several serious side effects, including pulmonary toxicity, thyroid dysfunction, and liver damage.
Choice B rationale:
Lidocaine is another antiarrhythmic medication that is sometimes used to treat ventricular arrhythmias. However, it is also not the first-line drug for Torsades de Pointes.
Lidocaine is less likely to worsen QT prolongation than amiodarone, but it can still have this effect in some patients.
Additionally, lidocaine has a short half-life and must be given as a continuous infusion, which can be challenging in a critical care setting.
Choice C rationale:
Atropine is a medication that is used to increase heart rate. It is not effective in treating Torsades de Pointes and is not indicated in this situation.
Atropine works by blocking the vagus nerve, which slows heart rate. In Torsades de Pointes, the heart rate is already very fast, so atropine would not be helpful.
Additionally, atropine can have several side effects, including dry mouth, blurred vision, and urinary retention.
Choice D rationale:
Magnesium sulfate is the first-line drug for treating Torsades de Pointes. It works by stabilizing the electrical activity of the heart and preventing further episodes of arrhythmia.
Magnesium sulfate is a relatively safe medication with few side effects. It can be given as an intravenous infusion or as an intramuscular injection.
Studies have shown that magnesium sulfate is effective in terminating Torsades de Pointes and preventing recurrences.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A rationale:
Severe acidemia: A pH of 6.9 indicates severe acidemia, a condition where the blood is too acidic. Sodium bicarbonate is an alkalizing agent that can help raise the blood pH back to a normal range.
Rapid correction: Intravenous (IVP) administration of sodium bicarbonate allows for rapid correction of acidemia, which is crucial in severe cases to prevent life-threatening complications.
Buffering action: Sodium bicarbonate acts as a buffer, accepting excess hydrogen ions (H+) in the blood and converting them into water and carbon dioxide (CO2), which can be exhaled.
Specific indications: Sodium bicarbonate is typically used in cases of severe acidemia caused by metabolic acidosis, such as diabetic ketoacidosis or lactic acidosis. It may also be considered in cases of respiratory acidosis, but other interventions like ventilatory support are often prioritized.
Choice B rationale:
Calcium carbonate is not a direct treatment for acidemia: It is primarily used as an antacid to neutralize stomach acid and as a calcium supplement for bone health. While it can have a mild alkalizing effect, it is not as effective as sodium bicarbonate in rapidly correcting severe acidemia.
Choice C rationale:
Alkalemia: A pH of 7.6 indicates alkalemia, a condition where the blood is too alkaline. Administration of sodium bicarbonate in this situation would worsen the alkalemia and potentially lead to serious complications.
Choice D rationale:
Hyponatremia: Low serum sodium levels do not directly require treatment with sodium bicarbonate. Sodium bicarbonate is primarily used to address acid-base imbalances, not electrolyte imbalances.
Correct Answer is D
Explanation
Choice A rationale:
Stevens-Johnson syndrome (SJS) is a rare, serious skin condition that is typically caused by an allergic reaction to medication. While amiodarone has been associated with a few cases of SJS, it is not considered a common long-term side effect.
Choice B rationale:
Ventricular tachycardia (VT) is a type of fast heart rhythm that originates in the ventricles of the heart. Amiodarone is actually used to treat VT, so it would be counterintuitive to list it as a long-term side effect.
Choice C rationale:
Pulmonary fibrosis is a condition characterized by scarring of the lung tissue. While amiodarone can cause pulmonary toxicity, which includes pulmonary fibrosis, this is a relatively rare side effect. Moreover, it's usually associated with high doses or
long-term use of the medication.
Choice D rationale:
QT prolongation is a condition in which the heart's electrical activity takes longer than normal to recharge between beats. This can lead to a potentially fatal arrhythmia called torsades de pointes. Amiodarone is known to prolong the QT interval, and this is considered one of its most significant long-term side effects. It's important to monitor patients on amiodarone for QT prolongation and to adjust the dose or discontinue the medication if necessary.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
