The practical nurse (PN) is assessing an older client with left-sided heart failure (HF). What intervention is most important for the PN to implement?
Inspect for sacral edema.
Measure urinary output.
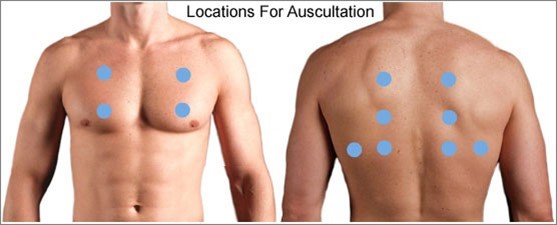
Auscultate all lung fields.
Check mental acuity.
The Correct Answer is C
When assessing an older client with left-sided heart failure (HF), the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. Left-sided heart failure is characterized by the inability of the left ventricle to effectively pump blood, leading to fluid accumulation in the lungs. Auscultating all lung fields allows the PN to assess for the presence of abnormal lung sounds such as crackles, indicating pulmonary congestion.
Let's evaluate the other options:
a) Inspect for sacral edema.
Sacral edema is commonly associated with right-sided heart failure, not left-sided heart failure. While it is important to assess for edema in clients with heart failure, inspecting for sacral edema may not be the most immediate and crucial intervention in this specific case.
b) Measure urinary output.
Measuring urinary output is a valuable assessment in many clinical situations, but it may not be the most vital intervention in the context of left-sided heart failure. Monitoring urinary output is more relevant in assessing kidney function and fluid balance rather than directly assessing the severity of left-sided heart failure.
d) Check mental acuity.
Checking mental acuity is important in assessing the overall condition of the client, but it is not the most crucial intervention specifically related to left-sided heart failure. Mental status evaluation is more useful in identifying signs of altered mental status or potential complications, rather than directly assessing the impact of left-sided heart failure.
In summary, when assessing an older client with left-sided heart failure, the most important intervention for the practical nurse (PN) to implement is to auscultate all lung fields. This allows for the detection of abnormal lung sounds associated with pulmonary congestion, a hallmark sign of left-sided heart failure.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A rationale:
Assessment of tobacco use geared toward adolescents. Rationale: While assessing tobacco use is essential for promoting health in adolescents, the question is about developing a class about mental health and addressing the increase in suicides in the community. Assessing tobacco use is not directly related to this topic. Stress self-management techniques are more relevant.
Choice B rationale:
Exploration of stress self-management techniques. Rationale: This is the correct answer. Addressing stress and teaching adolescents self-management techniques is crucial in the context of mental health promotion and suicide prevention. Adolescents often face stressors, and providing them with effective strategies to manage stress can contribute to their overall well-being.
Choice C rationale:
Video with statistics showing trends in suicide rates. Rationale: While providing statistics about suicide rates can be informative, it may not be the most engaging or effective method for teaching adolescents about mental health and stress management. Interactive activities and skill-building exercises are often more beneficial.
Choice D rationale:
Handouts for local substance abuse treatment centers. Rationale: Providing handouts for substance abuse treatment centers
Correct Answer is D
Explanation
Choice A rationale:
This statement is incorrect. Major Depressive Disorder (MDD) is typically more severe than dysthymia and is characterized by recurrent episodes of severe depression lasting at least two weeks.
Choice B rationale:
This statement is incorrect. Dysthymia is not characterized by alternating episodes of mania and depression. It is a chronic, low-grade depressive disorder.
Choice C rationale:
This statement is incorrect. Dysthymia can impair social and occupational functioning, similar to MDD. Both conditions can have a significant impact on a person's daily life.
Choice D rationale:
This statement is accurate. Dysthymia is a chronic depressive disorder that lasts for at least two years but is generally less severe than MDD. It is characterized by persistent, milder symptoms of depression.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
