The nurse is caring for a 10-year-old who has an acute head injury, has a pediatric Glasgow coma score of 9. and is unconscious. Which interventions should the nurse include in the child's care plan?
Elevate the head of the bed 15 to 30 degrees with head maintained a midline position.
Maintain an active stimulating environment
Perform active chest percussion and suctioning every 1 to 2 hours.
Instruct child on preforming active range of motion
The Correct Answer is A
A. Elevate the head of the bed 15 to 30 degrees with head maintained a midline position.
Correct Explanation: This intervention is appropriate for a child with an acute head injury.
Explanation: Elevating the head of the bed helps reduce intracranial pressure by facilitating venous drainage from the head. However, it's important to keep the head in a midline position to prevent neck flexion, which can obstruct venous flow. Elevating the head 15 to 30 degrees is a standard approach for managing intracranial pressure in patients with head injuries.
B. Maintain an active stimulating environment.
Incorrect Explanation: Maintaining an active stimulating environment is not suitable for a child with an acute head injury.
Explanation: A child with an acute head injury should be in a quiet and calm environment. Overstimulation can worsen the condition by increasing intracranial pressure. It's important to minimize stimuli to allow the brain to heal.
C. Perform active chest percussion and suctioning every 1 to 2 hours.
Incorrect Explanation: Chest percussion and suctioning are not relevant interventions for an acute head injury.
Explanation: Active chest percussion and suctioning are typically used to manage respiratory conditions. While maintaining good respiratory function is important for overall patient care, it's not a primary intervention for an unconscious child with a head injury.
D. Instruct child on performing active range of motion.
Incorrect Explanation: Instructing the child on performing active range of motion is not appropriate for an unconscious child with a head injury.
Explanation: An unconscious child cannot actively perform range of motion exercises. Additionally, it's not a priority intervention in the acute phase of head injury management.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
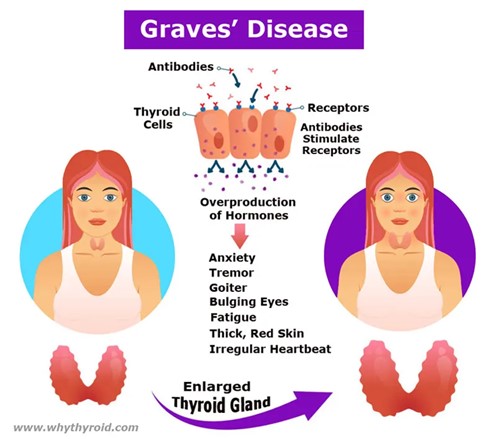
A) Heat intolerance.
Explanation: This statement is true. Heat intolerance is a common symptom of hyperthyroidism, including Graves' disease. People with hyperthyroidism often have an overactive thyroid gland that produces an excessive amount of thyroid hormones. This can lead to an increased metabolic rate, which in turn makes them sensitive to heat. They may feel excessively warm, sweat more than usual, and have difficulty tolerating hot weather.
B) Weight gain.
Explanation: This statement is false. Weight gain is not a typical finding in Graves' disease or hyperthyroidism. In fact, one of the hallmark symptoms of hyperthyroidism is unexplained weight loss despite increased appetite. The elevated levels of thyroid hormones cause an increase in metabolism, leading to weight loss.
C) Bradycardia.
Explanation: This statement is false. Bradycardia refers to an abnormally slow heart rate, typically below 60 beats per minute. In hyperthyroidism, the heart rate is often elevated rather than slowed down. The excessive thyroid hormones can lead to an increased heart rate (tachycardia) and palpitations. It's important to note that if the question were about hypothyroidism (underactive thyroid), bradycardia might be more relevant.
D) Lethargy.
Explanation: This statement is false. Lethargy, or a state of extreme tiredness and lack of energy, is more commonly associated with hypothyroidism (underactive thyroid) rather than hyperthyroidism. Hyperthyroidism usually leads to symptoms of increased energy, restlessness, and hyperactivity due to the elevated metabolic rate caused by excess thyroid hormones.
Correct Answer is B
Explanation
A. Dizziness is always a sign of a concussion.
This statement is incorrect. While dizziness can be a symptom of a concussion, it is not always indicative of a concussion. There can be various causes of dizziness, and it is essential to consider other symptoms as well when assessing for a concussion.
B. Bike Helmet Safety
Explanation:
The correct answer to include as part of concussion/head injury prevention teaching to children and parents is "Bike helmet safety." This is because wearing a helmet while riding a bike or participating in other activities that involve head injury risks is crucial to prevent head injuries and concussions. Helmets provide protection to the head by absorbing impact energy and reducing the risk of skull fractures or traumatic brain injuries.
C. Normal fluid intake.
While staying hydrated is important for overall health, it is not directly related to concussion or head injury prevention teaching. This choice is unrelated to the topic.
D. Signs of autism.
Signs of autism are unrelated to concussion or head injury prevention teaching. This choice is not relevant to the topic at hand.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
