A nurse in a provider’s office is caring for a client who is at 34 weeks of gestation and at risk for placental abruption. The nurse should recognize that which of the following is the most common risk factor for abruption?
Cocaine use
Blunt force trauma
Hypertension
Cigarette smoking
The Correct Answer is C
Choice A reason:
Cocaine use: Cocaine use during pregnancy is a significant risk factor for placental abruption. Cocaine causes vasoconstriction, which can reduce blood flow to the placenta and lead to its premature separation from the uterine wall. However, it is not the most common risk factor.
Choice B reason:
Blunt force trauma: Trauma to the abdomen, such as from a car accident or a fall, can cause placental abruption. This type of trauma can lead to the separation of the placenta from the uterine wall, resulting in bleeding and potential complications for both the mother and the fetus.
Choice C reason:
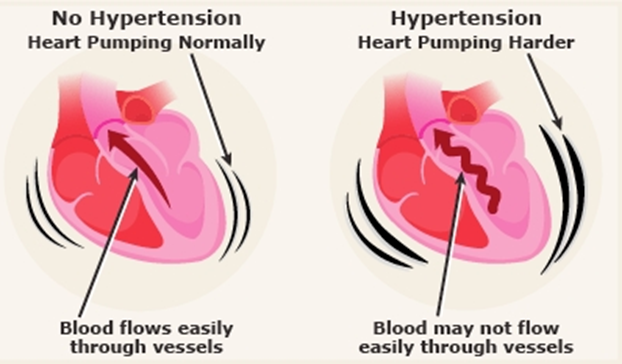
Hypertension: Hypertension, or high blood pressure, is the most common risk factor for placental abruption. Chronic hypertension or pregnancy-induced hypertension (preeclampsia) can damage the blood vessels in the placenta, leading to its premature separation. This condition can significantly increase the risk of placental abruption and is a critical factor to monitor in pregnant women.
Choice D reason:
Cigarette smoking: Smoking during pregnancy is another risk factor for placental abruption. Nicotine and other harmful substances in cigarettes can affect placental blood flow and increase the risk of abruption. However, like cocaine use, it is not the most common risk factor.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A reason:
Preparing the newborn for transport to the NICU is unnecessary in this scenario. An apical heart rate of 130 beats per minute (bpm) is within the normal range for a newborn, which typically falls between 100 and 170 bpm. Transporting the newborn to the NICU would be appropriate if there were other signs of distress or abnormal findings, but not solely based on a heart rate of 130 bpm.
Choice B reason:
Calling the provider to further assess the newborn is not required in this case. Since the heart rate of 130 bpm is within the normal range for a newborn, there is no immediate need for further assessment by the provider. This action would be more appropriate if the heart rate were outside the normal range or if there were other concerning symptoms.
Choice C reason:
Asking another nurse to verify the heart rate is also unnecessary. The heart rate of 130 bpm is within the expected range for a newborn, so there is no need for additional verification. This step might be taken if there were doubts about the accuracy of the initial measurement or if the heart rate were abnormal.
Choice D reason:
Documenting this as an expected finding is the correct action. A heart rate of 130 bpm is normal for a newborn, and it should be recorded as such in the newborn’s medical records. Proper documentation ensures accurate tracking of the newborn’s health status and helps in monitoring any changes over time.
Correct Answer is B
Explanation
Choice A Reason:
The Apgar score is a quick test performed on a newborn at 1 and 5 minutes after birth. The 5 criteria assessed are Appearance (skin color), Pulse (heart rate), Grimace response (reflexes), Activity (muscle tone), and Respiration (breathing effort). Each criterion is scored on a scale of 0 to 2, with 2 being the best score. The total score is calculated by adding the scores of all five criteria, with a maximum possible score of 10.
For this newborn:
• Appearance: The newborn has a pink trunk and head but bluish hands and feet, which scores 1 point12.
• Pulse: The heart rate is 130/min, which scores 2 points1.
• Grimace: The newborn has a weak, slow cry, which scores 1 point3.
• Activity: The newborn has flexed extremities, which scores 1 point3.
• Respiration: The newborn has a weak, slow cry, which scores 1 point3.
Adding these scores: 1 (Appearance) + 2 (Pulse) + 1 (Grimace) + 1 (Activity) + 1 (Respiration) = 6.
Choice B Reason:
This choice is correct. As explained above, the total Apgar score for this newborn is 6. The breakdown of the scores is as follows:
• Appearance: 1 point for pink trunk and head, bluish hands and feet.
• Pulse: 2 points for a heart rate of 130/min.
• Grimace: 1 point for a weak, slow cry.
• Activity: 1 point for flexed extremities.
• Respiration: 1 point for a weak, slow cry.
Choice C Reason:
This choice is incorrect. A score of 7 would require higher scores in one or more of the criteria. For example, if the newborn had a strong cry (2 points for Grimace and Respiration) or if the entire body was pink (2 points for Appearance), the total score would be higher.
Choice D Reason:
This choice is incorrect. A score of 8 would require even higher scores in the criteria. For instance, if the newborn had a strong cry and the entire body was pink, the total score would be 8 or higher.
Choice E Reason:
This choice is incorrect. A score of 9 would require almost perfect scores in all criteria, which is not the case for this newborn. The newborn’s weak, slow cry and bluish hands and feet lower the total score.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
