A client with nasal congestion receives a prescription for phenylephrine 10 mg PO every 4 hours. Which client condition should the nurse report to the healthcare provider before administering the medication?
Bronchitis.
Diarrhea.
Hypertension.
Edema.
The Correct Answer is C
Choice A Reason:
Bronchitis is a condition that affects the respiratory system, and while it is important to monitor, it is not a primary concern when administering phenylephrine. Phenylephrine is a decongestant that works by narrowing the blood vessels in the nasal passages, which can help relieve congestion but does not directly impact bronchitis.
Choice B Reason:
Diarrhea is a gastrointestinal condition that, while uncomfortable, does not significantly interact with phenylephrine. It is important to manage and monitor, but it does not pose a direct risk when taking phenylephrine.
Choice C Reason:
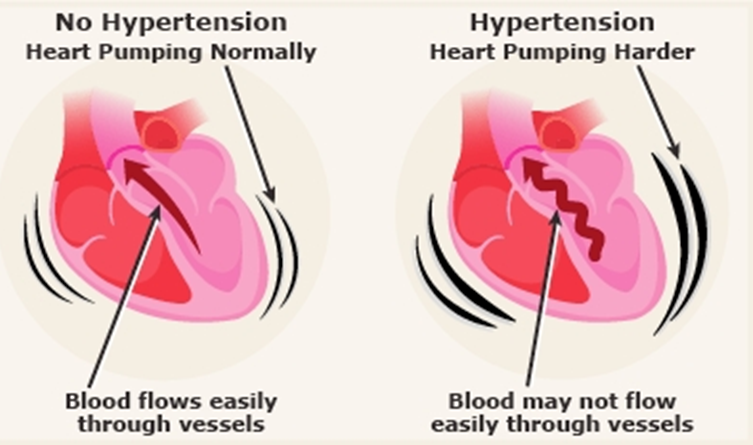
Hypertension is a significant concern when administering phenylephrine. Phenylephrine can increase blood pressure by causing vasoconstriction. For clients with hypertension, this can exacerbate their condition and lead to serious cardiovascular complications. Therefore, it is crucial to report this condition to the healthcare provider before administering the medication.
Choice D Reason:
Edema, or swelling, can be a symptom of various underlying conditions, including heart failure or kidney issues. While it is important to monitor, it is not as directly impacted by phenylephrine as hypertension. However, any underlying condition causing edema should be considered when administering medications.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason:
Accommodation refers to the eye’s ability to change the shape of the lens to focus on objects at different distances. Mydriatic eye drops primarily affect the muscles that control the pupil size, not the lens. While accommodation might be slightly affected due to the dilation, it is not the primary function impacted by mydriatics.
Choice B Reason:
Refraction is the bending of light as it passes through the lens of the eye to focus on the retina. Mydriatic eye drops do not directly affect the refractive properties of the eye. The primary purpose of these drops is to dilate the pupil, which does not significantly alter the eye’s refractive ability.
Choice C Reason:
Eye convergence is the simultaneous inward movement of both eyes toward each other to maintain single binocular vision when viewing an object. Mydriatic eye drops do not directly interfere with the muscles responsible for eye convergence. Therefore, this function remains largely unaffected during the therapeutic period.
Choice D Reason:
Pupillary constriction is the narrowing of the pupil, which is controlled by the sphincter pupillae muscle. Mydriatic eye drops cause the pupil to dilate by relaxing this muscle, thereby preventing pupillary constriction. This is the primary function that will not respond during the therapeutic period after administration of mydriatic eye drops.
Correct Answer is {"A":{"answers":"A"},"B":{"answers":"A"},"C":{"answers":"A"},"D":{"answers":"B"},"E":{"answers":"C"},"F":{"answers":"A"}}
Explanation
Choice A: Capillary refill 2 seconds
Reason: Capillary refill time is a quick test to assess peripheral perfusion and hydration status. A normal capillary refill time is less than 2 seconds. Initially, the patient had a capillary refill time of 5 seconds, indicating poor perfusion, likely due to dehydration from vomiting and diarrhea. After the administration of IV fluids and sodium bicarbonate, the capillary refill time improved to 2 seconds, which is within the normal range. This improvement indicates that the treatment was effective in restoring adequate perfusion and hydration, making it a therapeutic result.
Choice B: Blood pressure 113/72 mm Hg
Reason: Normal blood pressure for adults is typically around 120/80 mm Hg. The patient’s initial blood pressure was 100/77 mm Hg, which is on the lower side, likely due to dehydration. After receiving IV fluids and sodium bicarbonate, the blood pressure improved to 113/72 mm Hg, which is closer to the normal range. This indicates that the treatment helped to stabilize the patient’s blood pressure, making it a therapeutic result.
Choice C: Bicarbonate 22 mEq/L (22 mmol/L)
Reason: The normal range for bicarbonate (HCO3) is 21 to 28 mEq/L. The patient’s initial bicarbonate level was 15 mEq/L, indicating metabolic acidosis, likely due to severe vomiting and diarrhea. After the administration of sodium bicarbonate, the bicarbonate level increased to 22 mEq/L, which is within the normal range. This indicates that the sodium bicarbonate effectively corrected the metabolic acidosis, making it a therapeutic result.
Choice D: Sodium 152 mEq/L (152 mmol/L)
Reason: The normal range for sodium is 135 to 145 mEq/L. The patient’s sodium level of 152 mEq/L is above the normal range, indicating hypernatremia. This could be a non-therapeutic side effect of the sodium bicarbonate administration, as sodium bicarbonate can increase sodium levels in the blood. Hypernatremia can lead to symptoms such as confusion, muscle twitching, and seizures, and requires careful monitoring and management.
Choice E: 400 mL urine output
Reason: The patient’s urine output of 400 mL is not directly related to the administration of sodium bicarbonate. Urine output is influenced by various factors, including fluid intake, kidney function, and overall hydration status. In this case, the urine output is more likely related to the patient’s overall fluid balance and hydration status rather than a direct effect of the sodium bicarbonate. Therefore, it is considered an unrelated finding.
Choice F: Heart rate 77 beats/minute
Reason: A normal resting heart rate for adults ranges from 60 to 100 beats per minute. The patient’s initial heart rate was 102 beats per minute, which is elevated, likely due to dehydration and metabolic acidosis. After receiving IV fluids and sodium bicarbonate, the heart rate decreased to 77 beats per minute, which is within the normal range. This indicates that the treatment helped to stabilize the patient’s heart rate, making it a therapeutic result.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
