Here is the edited text:
An older client recently transferred to a rehabilitation facility after aortic valve replacement surgery is experiencing anxiety and difficulty adjusting to the transition. The healthcare provider prescribes an antidepressant and a mild sedative for sleep. Which intervention is most important for the nurse to include in the client's plan of care?
Obtain a blood pressure reading before the client gets out of bed.
Monitor and record the client's urinary output every day.
Provide the client with teaching regarding a cardiac diet.
Assess the client's vital signs every 4 hours when awake.
The Correct Answer is A
Choice A: Obtain a blood pressure reading before the client gets out of bed. This is the most important intervention, as it can prevent or detect orthostatic hypotension, which is a drop in blood pressure when changing position from lying to standing. Orthostatic hypotension can cause dizziness, fainting, or falls, and it can be caused by medications, dehydration, or cardiac problems.
Choice B: Monitor and record the client's urinary output every day. This is not the most important intervention, as it does not address the client's anxiety or adjustment issues. The urinary output should be monitored for signs of fluid balance, kidney function, or infection, but it is not a priority for this client.
Choice C: Provide the client with teaching regarding a cardiac diet. This is not the most important intervention, as it does not address the client's anxiety or adjustment issues. The cardiac diet should be taught to promote heart health, lower cholesterol, and reduce sodium intake, but it is not a priority for this client.
Choice D: Assess the client's vital signs every 4 hours when awake. This is not the most important intervention, as it does not address the client's anxiety or adjustment issues. The vital signs should be assessed for signs of infection, pain, or hemodynamic instability, but they are not a priority for this client.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A: Which medication works best for you? This is not the most important question, as it does not address the current status or risk of the client. The medication history is a part of the assessment, but it does not help identify the content or impact of the hallucinations.
Choice B: When do you hear voices? This is not the most important question, as it does not address the current status or risk of the client. The frequency and timing of the hallucinations are a part of the assessment, but they do not help identify the content or impact of the hallucinations.
Choice C: How do you cope with the voices? This is not the most important question, as it does not address the current status or risk of the client. The coping strategies are a part of the assessment, but they do not help identify the content or impact of the hallucinations.
Choice D: What are the voices saying? This is the most important question, as it addresses the current status and risk of the client. The content and impact of the hallucinations are a part of the assessment, as they can help identify if the client is experiencing command hallucinations, which may instruct them to harm themselves or others.
Correct Answer is C
Explanation
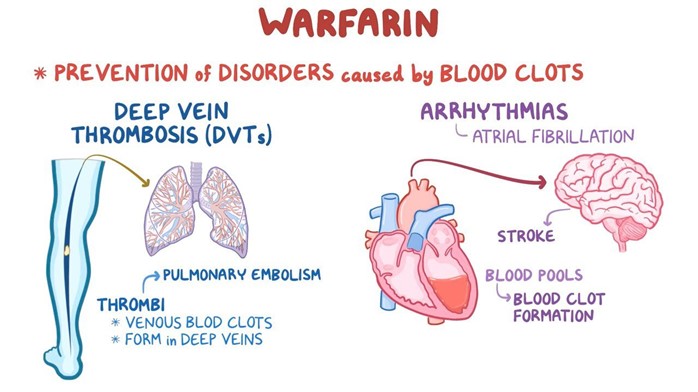
Choice A reason: Increasing the intake of dark green leafy vegetables while taking warfarin is not a good instruction because it can decrease the effectiveness of warfarin. Dark green leafy vegetables are rich in vitamin K, which is a coagulation factor that counteracts the anticoagulant effect of warfarin.
Choice B reason: Eating two servings of dark green leafy vegetables daily and continuing for 30 days after warfarin therapy is completed is not a good instruction because it can cause bleeding complications. Dark green leafy vegetables are rich in vitamin K, which is a coagulation factor that counteracts the anticoagulant effect of warfarin. Stopping warfarin while continuing to eat high amounts of vitamin K can increase the risk of clot formation and thromboembolism.
Choice D reason: Avoiding eating any foods that contain any vitamin K because it is an antagonist of warfarin is not a good instruction because it can cause bleeding complications. Dark green leafy vegetables are rich in vitamin K, which is a coagulation factor that counteracts the anticoagulant effect of warfarin. Eliminating vitamin K from the diet can increase the sensitivity to warfarin and cause excessive bleeding and bruising.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
