A primary healthcare provider prescribes 14 units of insulin to a client.
What should a nurse do while administering this medication to the client?
Administer 14 units of medication SubQ in a U-100 syringe
Administer 14 units of medication SubQ in two divided doses in a U-100 syringe
Administer 14 units of medication SubQ in one dose in a tuberculin syringe
Administer 14 units of medication SubQ in the morning after breakfast in a tuberculin syringe
The Correct Answer is A
Insulin is a hormone that helps regulate blood sugar levels. It is usually injected into the fat layer just under the skin (subcutaneous or SubQ) using a syringe and needle or a pen-like device². Insulin syringes are marked in units of insulin, not milliliters or cubic centimeters. The most common insulin syringe holds 1 mL of fluid and has markings for 100 units of insulin². A U-100 syringe means that for every 1 mL of fluid, there are 100 units of insulin³.
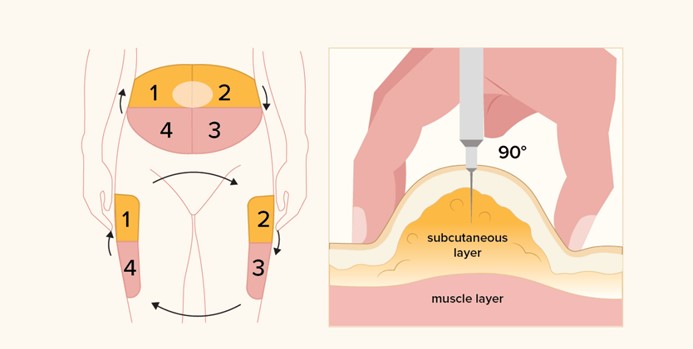
To administer 14 units of insulin, you would need to draw up 0.14 mL of fluid in a U-100 syringe. You would inject the insulin into your abdomen, upper arm, butocks, hip, or the front or side of the thigh¹. You would use a different area within the site each time you inject insulin to prevent lumps, swelling, or thickened skin¹.
The other options are incorrect because:
b) There is no need to divide the dose into two injections. This would increase the risk of infection and pain.
c) A tuberculin syringe is not designed for insulin administration. It is marked in milliliters or cubic centimeters, not units of insulin. Using a tuberculin syringe could result in an incorrect dose of insulin.
d) The timing of insulin administration depends on the type and duration of insulin. Some insulins are taken before meals, some are taken after meals, and some are taken once or twice a day. The primary healthcare provider should specify when to take the insulin.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
This statement is correct because the abdomen has a large surface area and a good blood supply, which allows for a consistent and predictable absorption of insulin. Insulin is a hormone that regulates blood glucose levels and needs to be delivered in precise doses to avoid complications such as hypoglycemia (low blood glucose) or hyperglycemia (high blood glucose).
The abdomen is also easy to access and has less variation in fat thickness, which reduces the risk of injecting into the muscle or the skin instead of the subcutaneous tissue. The subcutaneous tissue is the layer of fat and connective tissue below the skin and above the muscle, where insulin injections are given.
The other statements are not correct because they do not explain why the abdomen is the preferred site for subcutaneous insulin injections or they contain false information.
a.It is the least painful location for this injection. This statement is false because pain is subjective and depends on many factors, such as the type and size of the needle, the technique and speed of injection, the temperature and viscosity of the insulin, and the individual's pain tolerance and sensitivity. The abdomen may not be the least painful location for everyone, and some people may prefer other sites, such as the arms, thighs, or butocks.
b.There are fewer insulin side effects when given in this site. This statement is false because insulin side effects are not related to the site of injection, but to the dose, type, and timing of insulin, as well as the individual's response to insulin and other factors, such as diet, exercise, stress, illness, and medications. Insulin side effects may include hypoglycemia, weight gain, allergic reactions, lipodystrophy (changes in fat tissue), or edema (swelling).
c.It causes less bruising at the site. This statement is false because bruising is caused by bleeding under the skin due to damage to blood vessels during injection. Bruising can occur at any site of injection and depends on many factors, such as the type and size of the needle, the technique and speed of injection, the pressure applied after injection, the individual's clotting ability and blood thinning medications, and the presence of any underlying conditions that affect blood vessels or circulation.
Correct Answer is D
Explanation
The correct technique for preparing this insulin order is to follow these steps¹²:
- Perform hand hygiene and put on gloves.
- Mix NPH (cloudy) insulin by gently rotating the vial between the palms of your hands. Do not shake the vial.
- Clean the tops of both vials with alcohol swabs and let them dry.
- Draw up the amount of air equal to the dose of NPH insulin into a syringe. Inject the air into the NPH vial without touching the needle to the solution. Withdraw the needle and syringe without drawing up any insulin. This will create positive pressure in the NPH vial and make it easier to draw up later.
- Draw up the amount of air equal to the dose of regular (clear) insulin into the same syringe. Inject the air into the regular vial and invert the vial. Make sure the needle tip is below the fluid level and draw up slightly more than the dose of regular insulin. Tap the syringe gently to remove any air bubbles and push out any excess insulin to get the exact dose. Withdraw the needle and syringe from the regular vial.
- Reinsert the needle and syringe into the NPH vial without touching the needle to the solution. Invert the vial and draw up slightly more than the dose of NPH insulin. Tap the syringe gently to remove any air bubbles and push out any excess insulin to get the exact dose. Withdraw the needle and syringe from the NPH vial.
- Check that you have the correct doses of both insulins in one syringe. The total volume should be equal to the sum of both doses.
- Administer the dose within 5 to 10 minutes after drawing up because regular insulin binds to NPH and this decreases its action.

Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
