A patient with atrial fibrillation and a serum potassium level of 3.0 mEq/L takes digoxin (Lanoxin), ASA (aspirin), KCL (potassium chloride), and warfarin (Coumadin) daily. The patient reports visual disturbances. The nurse suspects problems with which medication?
Potassium chloride.
Warfarin.
Aspirin.
Digoxin.
The Correct Answer is D
Digoxin. Choice A rationale:
Potassium chloride (KCL) is a supplement used to treat or prevent low potassium levels. While it can have side effects, visual disturbances are not typically associated with KCL. Therefore, it is not the medication the nurse suspects to be causing the problem.
Choice B rationale:
Warfarin (Coumadin) is an anticoagulant used to prevent blood clot formation. Visual disturbances are not a known side effect of warfarin. Therefore, it is unlikely to be the cause of the patient's symptoms.
Choice C rationale:
Aspirin (ASA) is a pain reliever and antiplatelet medication, and while it can cause visual disturbances in some cases, it is not a common or significant side effect. Aspirin is also not specifically linked to atrial fibrillation.
Choice D rationale:

Digoxin (Lanoxin) is used to treat atrial fibrillation and heart failure. Visual disturbances are a known side effect of digoxin toxicity. Given the patient's diagnosis of atrial fibrillation and the reported symptoms, the nurse suspects the problem lies with digoxin and should further investigate and report to the provider.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Cerebral bleeding. Choice A rationale:
Stress fractures are not directly related to hypernatremia. Hypernatremia is an electrolyte imbalance, and its main effects are related to cellular dehydration and neurological symptoms rather than bone fractures.
Choice B rationale:
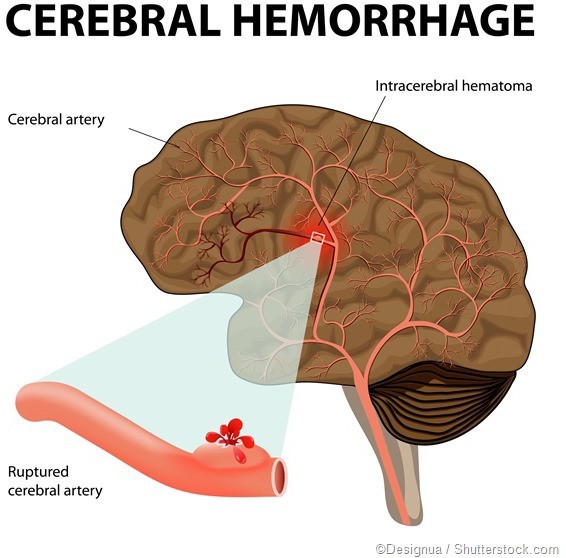
This is the correct answer because hypernatremia can lead to severe dehydration and cause neurological complications, including cerebral bleeding. The brain cells can shrink due to water loss, causing blood vessels to rupture, leading to bleeding in the brain.
Choice C rationale:
Atrial dysrhythmias are not directly associated with hypernatremia. Hypernatremia primarily affects the central nervous system and can lead to neurological symptoms rather than cardiac dysrhythmias.
Choice D rationale:
Pulmonary edema is not a likely consequence of hypernatremia. Pulmonary edema is associated with fluid volume excess, not fluid volume deficit, which is characteristic of hypernatremia.
Correct Answer is C
Explanation
Choice A rationale:
Sodium level is a laboratory parameter that can be helpful in assessing fluid balance, but it does not directly measure fluid retention. Abnormal sodium levels may indicate fluid imbalances, but it is not the most reliable measure of fluid retention.
Choice B rationale:
Tissue turgor refers to the skin's elasticity, and it can be used to assess dehydration rather than fluid retention. Poor turgor may indicate dehydration, but it does not specifically measure fluid volume increase.
Choice C rationale:
Daily weight is a reliable measure of fluid retention. An increase in weight over a short period may indicate fluid accumulation in the body, while a decrease in weight could signify fluid loss. It is essential to monitor weight consistently under standardized conditions (e.g., same time, same clothing) for accurate assessment.
Choice D rationale:
Intake and output records provide information about fluid intake and output but may not always reflect fluid retention accurately. It is helpful for assessing fluid balance, but daily weight is a more direct and reliable measure of fluid retention.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
