A nurse is reviewing discharge medications with a client who has Parkinson's disease. The nurse should include teaching about the client's anticholinergic agent. Which of the following side effects should the nurse advise the client to report?
Drooling
Anhidrosis
Tremors
Rigidity
The Correct Answer is B
Choice A Reason:
Drooling is inappropriate. Drooling, also known as sialorrhea, is a common symptom in Parkinson's disease due to impaired swallowing and reduced control of the muscles involved in saliva production. Anticholinergic medications can exacerbate dry mouth, which may contribute to drooling. However, drooling is not typically a side effect that would be specifically associated with anticholinergic use.
Choice B Reason:
Anhidrosis is appropriate. Anhidrosis refers to the inability to sweat normally. Anticholinergic medications can inhibit sweating by blocking the action of acetylcholine on sweat glands, leading to decreased sweating and potentially causing hyperthermia. Anhidrosis is a potential side effect of anticholinergic agents and should be reported to the healthcare provider due to the risk of overheating.
Choice C Reason:
Tremors is inappropriate. Tremors are a common symptom of Parkinson's disease and are typically not caused by anticholinergic medications. In fact, anticholinergic agents are often prescribed to help reduce tremors in individuals with Parkinson's disease. Tremors would not be considered an adverse effect that the client should report in the context of anticholinergic therapy.
Choice D Reason:
Rigidity is inappropriate. Rigidity, or stiffness of the muscles, is a characteristic symptom of Parkinson's disease resulting from the loss of dopamine-producing neurons in the brain. While anticholinergic medications can help alleviate some symptoms of Parkinson's disease, they are not typically associated with rigidity. Rigidity would not be considered an adverse effect that the client should report in the context of anticholinergic therapy.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A Reason:
Higher oxygen saturations of 98% to 99% is inappropriate. A pneumothorax involves the presence of air in the pleural space, which can compromise lung function and gas exchange. This compromised lung function typically leads to decreased oxygenation of the blood, resulting in lower oxygen saturations rather than higher saturations.
Choice B Reason:
Lower oxygen saturations of 93% to 94% is appropriate. A pneumothorax disrupts the normal exchange of oxygen and carbon dioxide in the lungs due to partial or complete lung collapse. As a result, the affected lung is unable to adequately oxygenate the blood, leading to lower oxygen saturations, which are indicative of hypoxemia.
Choice C Reason:
Lower energy expenditure is inappropriate. Energy expenditure is not typically affected by a pneumothorax. While the discomfort and respiratory distress associated with a pneumothorax may cause the individual to limit physical activity, there is no direct impact on overall energy expenditure.
Choice D Reason:
Increased lung capacity is inappropriate. A pneumothorax results in partial or complete collapse of the affected lung, reducing lung capacity rather than increasing it. The presence of air in the pleural space creates positive pressure, which can compress the lung and decrease its ability to expand fully during inhalation.
Correct Answer is ["B","D","E"]
Explanation
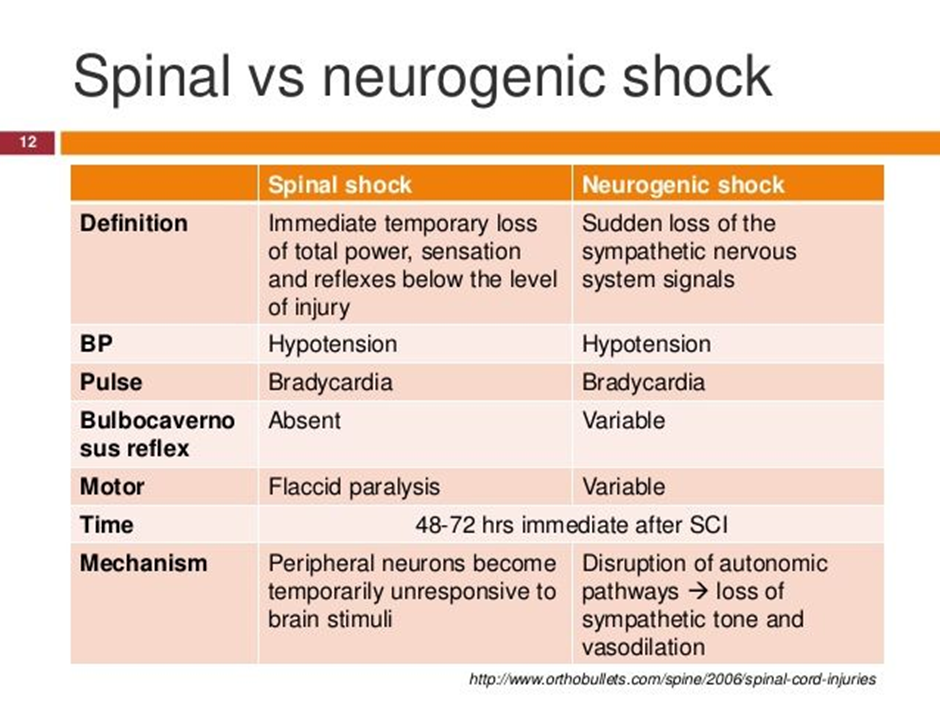
Choice A Reason:
Metoprolol is incorrect. Metoprolol is a beta-blocker medication commonly used to treat conditions such as hypertension, angina, and heart failure. However, in the context of neurogenic shock following a spinal cord injury, the use of beta-blockers such as metoprolol is generally contraindicated. Beta-blockers antagonize the effects of sympathetic activation, leading to a reduction in heart rate and myocardial contractility, which can exacerbate hypotension and bradycardia, the hallmarks of neurogenic shock. Therefore, the nurse would not anticipate a prescription for metoprolol in the management of neurogenic shock.
Choice B Reason:
Lactated Ringers intravenous fluid is correct. Fluid resuscitation with isotonic crystalloid solutions such as lactated Ringers is essential to restore intravascular volume and improve perfusion.
Choice C Reason:
Furosemide is incorrect. Furosemide is a loop diuretic medication commonly used to treat conditions such as heart failure, edema, and hypertension by promoting diuresis and reducing fluid volume. However, in the context of neurogenic shock, the use of diuretics such as furosemide is generally not indicated unless there is concurrent volume overload. Neurogenic shock is characterized by hypotension due to vasodilation and decreased systemic vascular resistance, often leading to relative hypovolemia rather than volume overload. Therefore, administering furosemide could further decrease intravascular volume, exacerbating hypotension and compromising perfusion. As a result, the nurse would not anticipate a prescription for furosemide in the management of neurogenic shock.:
Choice D Reason:
Dopamine is correct. Dopamine is a vasopressor medication that acts to increase vascular tone and blood pressure by stimulating alpha-adrenergic receptors. It is commonly used in the management of neurogenic shock to augment blood pressure.
Choice E Reason:
Epinephrine is correct. Epinephrine is a potent vasopressor that acts on both alpha and beta-adrenergic receptors, leading to vasoconstriction and increased cardiac output. It is used in the treatment of refractory hypotension in neurogenic shock.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
