A nurse is reinforcing teaching about a tonometry examination with a client who has manifestations of glaucoma. Which of the following statements should the nurse include in the teaching?
This test will measure the intraocular pressure of the eye.
Tonometry will allow inspection of the optic disc for signs of degeneration.
Tonometry is performed to evaluate peripheral vision.
This test will diagnose the type of your glaucoma.
The Correct Answer is A
Choice A Reason:
Tonometry is a diagnostic test that measures the intraocular pressure (IOP) inside the eye. This measurement is crucial for detecting and managing glaucoma, as elevated IOP is a significant risk factor for the disease. By measuring the pressure, healthcare providers can assess the risk of optic nerve damage and initiate appropriate treatments to prevent vision loss.
Choice B Reason:
Tonometry does not allow for the inspection of the optic disc for signs of degeneration. This function is typically performed using ophthalmoscopy or optical coherence tomography (OCT), which provide detailed images of the optic nerve and retina. These tests are essential for evaluating the structural damage caused by glaucoma but are not part of the tonometry procedure.
Choice C Reason:
Tonometry is not performed to evaluate peripheral vision. Peripheral vision is assessed using perimetry or visual field testing, which maps the field of vision and detects areas of vision loss. This test helps determine the extent of visual impairment caused by glaucoma but is separate from tonometry.
Choice D Reason:
Tonometry does not diagnose the type of glaucoma. While it measures intraocular pressure, diagnosing the specific type of glaucoma requires a comprehensive eye examination, including gonioscopy to examine the drainage angle of the eye and other tests to assess optic nerve health and visual field. Therefore, tonometry is just one component of the diagnostic process.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason:
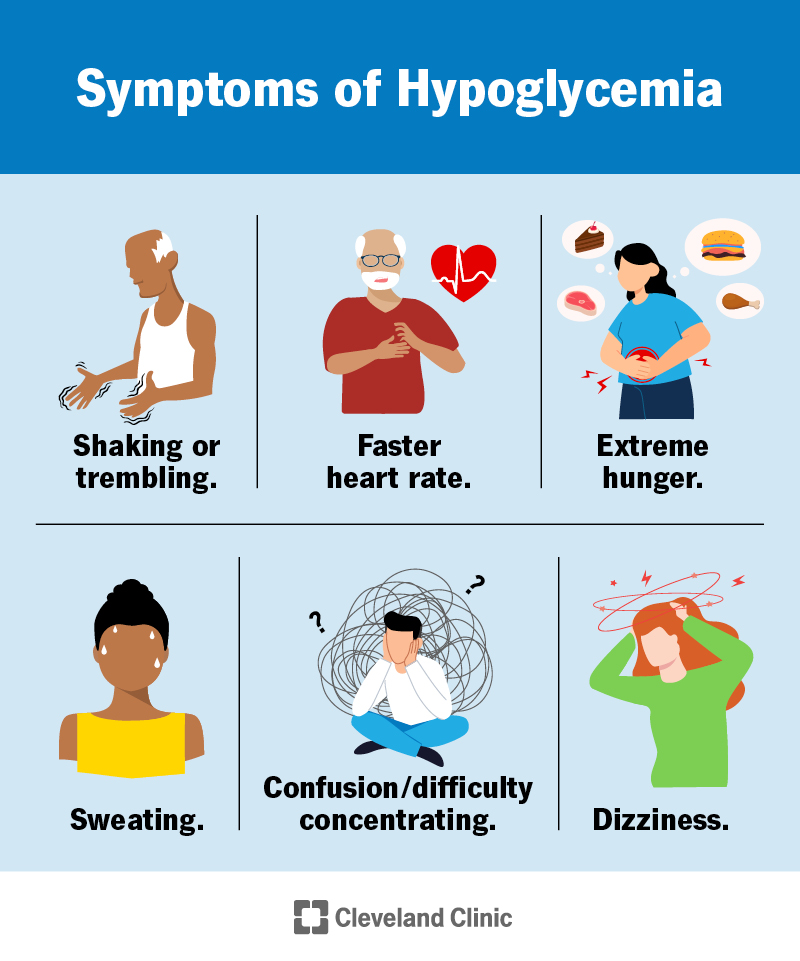
Warm and moist skin is not a typical manifestation of hypoglycemia. Instead, hypoglycemia often causes symptoms such as cold, clammy skin due to the body’s response to low blood sugar levels. Warm and moist skin can be associated with other conditions, such as hyperthyroidism or fever, but not hypoglycemia.
Choice B Reason:
A decreased appetite is not a common symptom of hypoglycemia. In fact, hypoglycemia can sometimes cause increased hunger as the body signals the need for more glucose. Symptoms of hypoglycemia are more related to the body’s immediate response to low blood sugar, such as shakiness, sweating, and confusion.
Choice C Reason:
Increased thirst is a symptom more commonly associated with hyperglycemia (high blood sugar) rather than hypoglycemia. When blood sugar levels are high, the body tries to eliminate excess glucose through urine, leading to dehydration and increased thirst. Hypoglycemia, on the other hand, does not typically cause increased thirst.
Choice D Reason:
Feeling shaky is a classic symptom of hypoglycemia. When blood sugar levels drop, the body releases adrenaline, which can cause shakiness, sweating, and a rapid heartbeat. Recognizing this symptom is crucial for individuals with diabetes to take immediate action to raise their blood sugar levels and prevent severe hypoglycemia.
Correct Answer is D
Explanation
Choice A Reason:
Primary hyperparathyroidism is characterized by elevated PTH levels, which lead to increased serum calcium levels and decreased serum phosphate levels. The patient’s lab results show low PTH and low serum calcium, which are not consistent with primary hyperparathyroidism.
Choice B Reason:
Chronic kidney disease (CKD) can cause disturbances in calcium and phosphate metabolism, but it typically presents with elevated PTH levels due to secondary hyperparathyroidism. The patient’s low PTH levels make CKD an unlikely diagnosis in this context.
Choice C Reason:
Vitamin D deficiency can lead to low serum calcium levels, but it usually results in elevated PTH levels as the body attempts to compensate for the low calcium. The patient’s low PTH levels do not align with a diagnosis of vitamin D deficiency.
Choice D Reason:
Hypoparathyroidism is characterized by low serum calcium, low PTH levels, and elevated serum phosphate levels. This condition occurs when the parathyroid glands do not produce enough PTH, leading to the observed lab results and symptoms such as tingling, muscle cramps, and fatigue. The patient’s lab results are consistent with hypoparathyroidism.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
