A nurse is providing teaching about the use of crutches using a three-point gait to a client who has a tibia fracture.
Which of the following actions by the client indicates an understanding of the teaching?
Moving both crutches with the stronger leg forward first.
Supporting his body weight while leaning on the axillary crutch pads
Stepping with his affected leg first when going up stairs
Positioning both hands on the grips with his elbows slightly flexed.
The Correct Answer is D
The correct answer is Choice d. Positioning both hands on the grips with his elbows slightly flexed.
Choice A rationale:
- Moving both crutches with the stronger leg forward first is incorrect for a three-point gait. This describes a two-point gait, which is used when a client can bear weight on both legs. In a three-point gait, the client bears weight on the unaffected leg and the crutches, not the stronger leg.
- This action would put excessive weight on the affected leg and could potentially compromise healing or cause further injury.
Choice B rationale:
- Supporting his body weight while leaning on the axillary crutch pads is also incorrect. This can lead to nerve damage in the armpits and should be avoided.
- The weight should be distributed through the hands and wrists, not the armpits.
Choice C rationale:
- Stepping with his affected leg first when going up stairs is incorrect and potentially dangerous. The client should lead with the stronger leg when going up stairs to maintain balance and control.
Choice D rationale:
- Positioning both hands on the grips with his elbows slightly flexed is the correct action for using crutches with a three-point gait. This allows for proper weight distribution, balance, and control of the crutches.
- It also helps to prevent fatigue and strain in the arms and shoulders.
Key points to remember about the three-point gait:
- Weight is borne on the unaffected leg and the crutches, not the affected leg.
- The crutches and the unaffected leg move forward together, followed by the affected leg.
- The client should look ahead, not down at their feet.
- The client should take small, even steps.
- The client should rest as needed.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
The correct answer is choice C: “Do you have thoughts of harming yourself?”.
This is the priority question for the nurse to ask the client because it assesses the client’s risk for suicide, which is a serious and potentially life-threatening complication of conduct disorder. The nurse should use a direct and nonjudgmental approach when asking about suicidal ideation and plan.
Choice A: “How do you get along with your peers at school?” is wrong because it is not the most urgent question to ask the client.
While it is important to assess the client’s social relationships and possible peer rejection, this can be done after addressing the client’s safety and mental status.
Choice B: “Do you have a criminal record?” is wrong because it is not relevant to the client’s current condition and might make the client feel defensive or stigmatized.
The nurse should avoid asking questions that imply blame or judgment and focus on the client’s strengths and coping skills.
Choice D: “How do you manage your behavior?” is wrong because it is not appropriate for the nurse to ask the client in an emergency department setting.
This question might imply that the client is responsible for their conduct disorder, which is a complex and multifactorial mental health condition. The nurse should collaborate with the client and their family to develop a behavior management plan that involves positive reinforcement, limit setting, and consistent consequences.
Normal ranges: According to the DSM-5, conduct disorder is characterized by a persistent pattern of behavior that violates the rights of others or societal norms.
The symptoms of conduct disorder include aggression, deceitfulness, destruction of property, serious rule violations, and lack of remorse.
Conduct disorder can cause significant impairment in social, academic, or occupational functioning. The prevalence of conduct disorder is estimated to be 4% among children and adolescents.
The risk factors for conduct disorder include genetic factors, neurobiological factors, environmental factors, and psychological factors.
Correct Answer is C
Explanation
This is a sign of preeclampsia, a serious complication of pregnancy that can cause high blood pressure, proteinuria, and seizures.
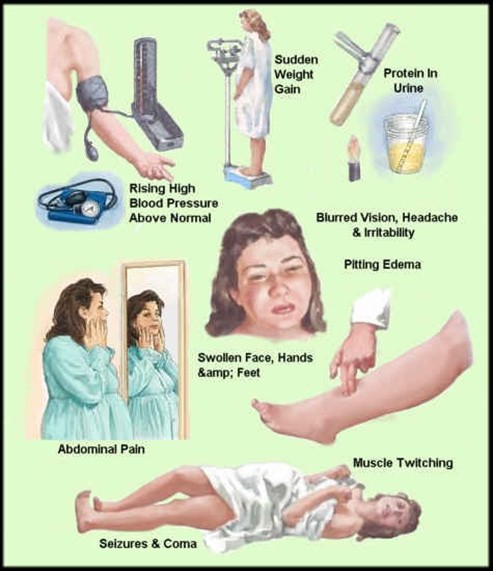
Preeclampsia can affect the placenta, the kidneys, the liver, and the brain of the mother and the fetus. It requires immediate medical attention and may lead to early delivery.
Choice A, bleeding gums, is wrong because it is a common occurrence during pregnancy due to hormonal changes that increase blood flow to the gums. It is not a cause for concern unless it is excessive or accompanied by other symptoms.
Choice B, urinary frequency, is wrong because it is also a normal finding during pregnancy due to the growing uterus putting pressure on the bladder. It is not a sign of infection or kidney problems unless it is associated with pain, burning, or blood in the urine.
Choice D, faintness upon rising, is wrong because it is usually caused by orthostatic hypotension, a drop in blood pressure when changing positions.
This can happen during pregnancy due to the dilation of blood vessels and the increased blood volume. It can be prevented by rising slowly, drinking enough fluids, and avoiding prolonged standing.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
