A nurse is planning care for a client who has a new prescription to receive a continuous infusion of total parenteral nutrition (TPN) Which of the following interventions should the nurse implement?
Change the TPN infusion tubing once every 3 days
Check the client's blood glucose level regularly
Insert the peripheral IV catheter for administration
Monitor the client's weight every 3 days
The Correct Answer is B
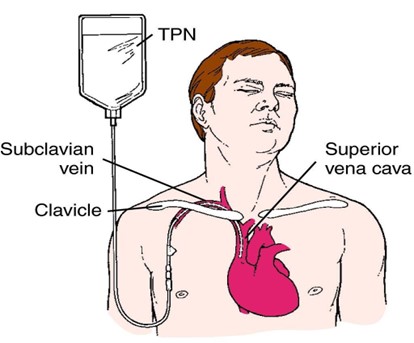
When caring for a client receiving a continuous infusion of total parenteral nutrition (TPN), the nurse should implement the intervention of checking the client's blood glucose level regularly. TPN is a highly concentrated intravenous nutrition solution containing glucose, amino acids, lipids, vitamins, and minerals, and it is used to provide complete nutrition when the client cannot take oral nutrition.
Monitoring blood glucose levels regularly is essential because TPN is rich in glucose, which can significantly affect the client's blood sugar levels. Hyperglycemia (high blood sugar) is a potential complication of TPN infusion. Regular blood glucose monitoring allows the nurse to detect and address any changes in blood sugar levels promptly and to adjust the TPN infusion rate or administer insulin, if necessary, to maintain the client's blood sugar within the target range.
Let's go through the other options:
A. Change the TPN infusion tubing once every 3 days: While changing the TPN infusion tubing regularly is a good practice to maintain asepsis and prevent infection, it is not the priority intervention in this situation. Regularly checking the client's blood glucose level is more crucial to monitor the effects of TPN on blood sugar levels.
C. Insert the peripheral IV catheter for administration: Total parenteral nutrition is a hypertonic solution that can cause irritation and damage to peripheral veins. It is usually administered through a central venous catheter (CVC) placed in a large vein, such as the subclavian or jugular vein. Inserting a peripheral IV catheter for TPN administration is not recommended due to the risk of vein damage and thrombosis.
D. Monitor the client's weight every 3 days: Monitoring the client's weight is an important part of assessing their nutritional status and fluid balance. However, the priority intervention for a client receiving TPN is checking their blood glucose level regularly, as hyperglycemia is a common and significant concern in TPN administration.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
When planning care for a client who had a myocardial infarction and is receiving thrombolytic therapy with an IV infusion of alteplase, the nurse should include the intervention of monitoring for changes in the client's level of consciousness.
Alteplase is a thrombolytic medication used to break down blood clots in certain medical emergencies, such as acute myocardial infarction (heart attack) or ischemic stroke. One of the potential complications of thrombolytic therapy, including alteplase, is bleeding. The medication's action of breaking down blood clots can also affect the body's natural clotting mechanisms, increasing the risk of bleeding.
Bleeding in the brain is a severe and potentially life-threatening complication associated with thrombolytic therapy. Therefore, it is essential for the nurse to closely monitor the client for any signs of intracranial bleeding, such as changes in the level of consciousness, confusion, severe headache, slurred speech, or weakness on one side of the body.
Let's go through the other options:
A. Administer aspirin instead of acetaminophen for fever: While aspirin is commonly used in the management of myocardial infarction, it is not specifically indicated for fever. Acetaminophen is the preferred antipyretic medication for fever management in most cases, and it does not interfere with the action of thrombolytic therapy.
B. Ambulate the client as often as tolerated: While early ambulation is beneficial for clients with myocardial infarction, it may not be appropriate during thrombolytic therapy. Thrombolytic therapy carries an increased risk of bleeding, and ambulation may be limited or contraindicated during the treatment period, depending on the client's overall condition and bleeding risk.
C. Administer a sodium phosphate enema for constipation: The administration of a sodium phosphate enema is not a specific intervention related to thrombolytic therapy or myocardial infarction. Bowel management is important for client comfort and overall well-being, but it is not a priority intervention in the immediate care of a client undergoing thrombolytic therapy.
Correct Answer is A
Explanation
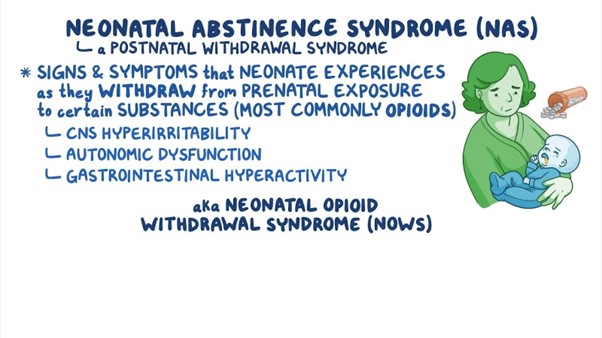
Neonatal abstinence syndrome (NAS) is a group of withdrawal symptoms that occur in newborns who were exposed to drugs, including heroin, in utero. Hyporeflexia, which refers to reduced or diminished reflexes, is one of the key findings in neonates experiencing NAS.
During pregnancy, when the mother uses opioids like heroin, the baby becomes dependent on the drug. After birth, when the drug is no longer available, the baby experiences withdrawal symptoms as the body adjusts to the absence of the drug. Hyporeflexia is a common manifestation of NAS and is observed due to the central nervous system's response to the withdrawal.
Let's go through the other options:
B. Frequent yawning: While yawning can be seen in neonates with NAS, it is not as specific to the condition as hyporeflexia. Yawning can occur for various reasons and may not always be indicative of NAS.
C. Respiratory depression: Respiratory depression can be a severe complication of opioid exposure in utero and can result in life-threatening situations for the neonate. However, it is not specific to NAS. Respiratory depression is more closely associated with opioid overdose in the newborn, which can be a separate concern from NAS.
D. Constipation: Constipation is a possible symptom in neonates experiencing NAS, but it is not as specific as hyporeflexia. Constipation can occur due to various factors and is not unique to NAS.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
