A client arrives to the clinic with reports of progressive weakness in his lower extremities. Which of the following findings in the client's history is consistent with the client developing Guillain-Barre syndrome?
Facial tumor
Pregnancy
Puncture wound 3 weeks ago
Cytomegalovirus
The Correct Answer is D
Choice A Reason: A facial tumor is not related to Guillain-Barre syndrome, which is an autoimmune disorder that affects the peripheral nerves.
Choice B Reason: Pregnancy is not a risk factor for Guillain-Barre syndrome, although it can occur during or after pregnancy in rare cases.
Choice C Reason: A puncture wound 3 weeks ago is unlikely to cause Guillain-Barre syndrome, which usually follows a respiratory or gastrointestinal infection.
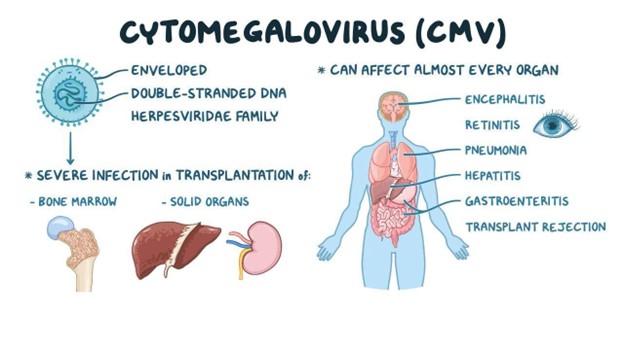
Choice D Reason: This is the correct answer because cytomegalovirus is one of the common infections that can trigger Guillain-Barre syndrome. It can cause inflammation and damage to the myelin sheath that covers the nerves.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A reason: This is incorrect because loss of peripheral vision is not a manifestation of cataracts, but of glaucoma. Glaucoma is a condition that causes increased pressure inside the eye and damage to the optic nerve, which can lead to loss of vision in the outer edges of the visual field. The nurse should assess the client's intraocular pressure and visual field test results to rule out glaucoma.
Choice B reason: This is correct because a decreased ability to perceive colors is a manifestation of cataracts. Cataracts are a condition that causes clouding or opacity of the lens, which is the transparent structure behind the pupil that focuses light onto the retina. Cataracts can reduce the clarity and contrast of vision and make colors appear faded or yellowish. The nurse should ask the client about any changes in color perception or brightness of objects.
Choice C reason: This is incorrect because loss of central vision is not a manifestation of cataracts but of macular degeneration. Macular degeneration is a condition that affects the macula, which is the central part of the retina that is responsible for sharp and detailed vision. Macular degeneration can cause blurred or distorted central vision, difficulty reading or recognizing faces, or dark spots in the visual field. The nurse should assess the client's visual acuity and fundoscopic examination results to rule out macular degeneration.
Choice D reason: This is incorrect because seeing bright flashes of light and floaters is not a manifestation of cataracts but of retinal detachment. Retinal detachment is a condition that occurs when the retina, which is the layer of tissue at the back of the eye that converts light into nerve impulses, separates from its underlying support tissue. Retinal detachment can cause sudden flashes of light, floaters, or shadows in the visual field. The nurse should refer the client to an ophthalmologist immediately if retinal detachment is suspected.
Correct Answer is A
Explanation
Choice A reason: This is correct because resuming a functional role in society is the ultimate goal for a client in the rehabilitative phase of a burn injury. The rehabilitative phase begins when wound healing is complete and lasts until physical and psychosocial recovery is achieved. The nurse should help the client regain independence, self-esteem, and quality of life by providing education, counseling, referrals, and resources.
Choice B reason: This is incorrect because pain management is not a goal, but an intervention for a client in the rehabilitative phase of a burn injury. Pain management is important throughout all phases of burn care, but especially during wound healing and scar formation, which can cause itching, tightness, or hypersensitivity. The nurse should assess the client's pain level and administer analgesics, antipruritics, or moisturizers as ordered.
Choice C reason: This is incorrect because providing continued full support to the client is not a goal, but an intervention for a client in the rehabilitative phase of a burn injury. Providing continued full support to the client can help them cope with physical and emotional challenges, such as scarring, disfigurement, disability, or depression. The nurse should provide emotional support, active listening, positive feedback, and encouragement to the client.
Choice D reason: This is incorrect because preventing infection is not a goal, but an intervention for a client in the rehabilitative phase of a burn injury. Preventing infection is crucial during wound healing and grafting, which can be compromised by bacterial colonization or contamination. The nurse should monitor the client's vital signs, wound appearance, and laboratory results, and administer antibiotics or antiseptics as ordered.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
