A 55-year-old female presents with symptoms of fatigue, muscle weakness, and depression. Laboratory results reveal elevated calcium levels and increased parathyroid hormone (PTH) levels. Which of the following is the most likely cause of her hyperparathyroidism?
Adenoma of the parathyroid gland.
Thyroid carcinoma.
Vitamin D deficiency.
Chronic kidney disease.
The Correct Answer is A
Choice A Reason:
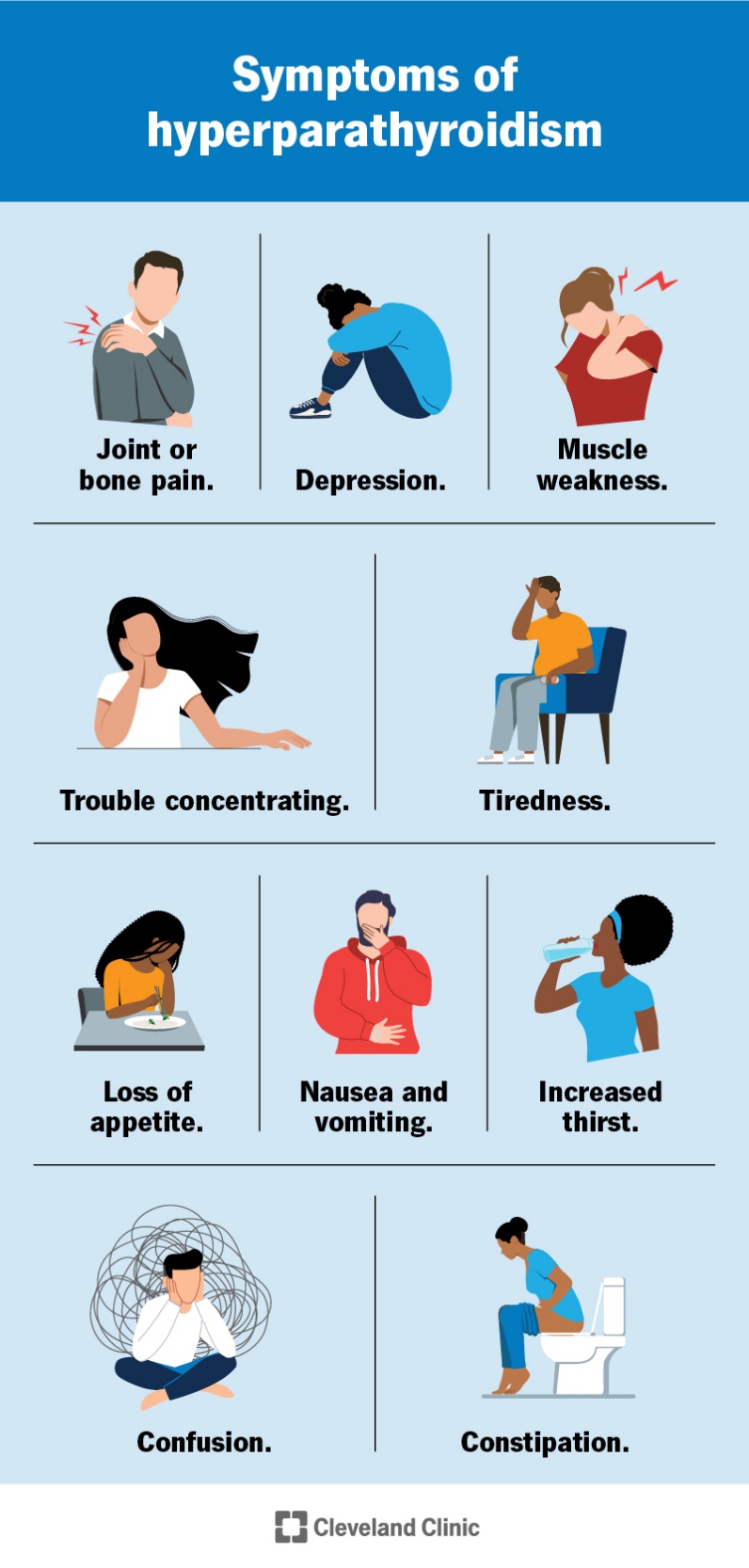
An adenoma of the parathyroid gland is the most common cause of primary hyperparathyroidism. This benign tumor leads to the overproduction of parathyroid hormone (PTH), which in turn causes elevated calcium levels in the blood. The excessive PTH secretion disrupts the normal calcium balance, leading to symptoms such as fatigue, muscle weakness, and depression. Parathyroid adenomas account for approximately 80% of primary hyperparathyroidism cases.
Choice B Reason:
Thyroid carcinoma is a type of cancer that originates in the thyroid gland, not the parathyroid glands. While thyroid carcinoma can cause various symptoms, it does not typically lead to elevated PTH levels or hyperparathyroidism. Therefore, it is not the most likely cause of the patient’s condition.
Choice C Reason:
Vitamin D deficiency can lead to secondary hyperparathyroidism, where low levels of vitamin D cause decreased calcium absorption, prompting the parathyroid glands to produce more PTH to maintain calcium levels. However, this condition is usually associated with low or normal calcium levels, not elevated calcium levels as seen in this patient. Therefore, it is not the most likely cause of her hyperparathyroidism.
Choice D Reason:
Chronic kidney disease (CKD) can also cause secondary hyperparathyroidism due to impaired kidney function, which affects calcium and phosphate balance and vitamin D metabolism. However, similar to vitamin D deficiency, CKD-related hyperparathyroidism typically presents with low or normal calcium levels rather than elevated levels. Thus, it is not the most likely cause in this scenario.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason:
Acute lymphoblastic leukemia (ALL) is a type of cancer that affects the blood and bone marrow. While it can cause symptoms such as fatigue and fever, it is less likely to cause severe pain in the lower back and joints, which are more characteristic of a vaso-occlusive crisis in sickle cell anemia. ALL typically presents with symptoms like frequent infections, easy bruising or bleeding, and bone pain, but the combination of severe pain, fatigue, and fever in a patient with sickle cell anemia points more towards a vaso-occlusive crisis.
Choice B Reason:
Iron-deficiency anemia is a condition where there is a lack of adequate iron to form healthy red blood cells. Symptoms include fatigue, weakness, and pale skin, but it does not typically cause severe pain in the lower back and joints or fever. The presence of severe pain and fever in a patient with sickle cell anemia is more indicative of a vaso-occlusive crisis rather than iron-deficiency anemia.
Choice C Reason:
Vaso-occlusive crisis is a common and painful complication of sickle cell anemia. It occurs when sickled red blood cells block blood flow to parts of the body, causing severe pain, often in the back, joints, and abdomen. This condition can also lead to fever and fatigue due to the body’s inflammatory response and the reduced oxygen delivery to tissues. Given the patient’s history of sickle cell anemia and the described symptoms, a vaso-occlusive crisis is the most likely cause.
Choice D Reason:
Pneumonia is an infection that inflames the air sacs in one or both lungs, which can cause symptoms such as fever, chills, and difficulty breathing. While pneumonia can occur in patients with sickle cell anemia, it is less likely to cause severe pain in the lower back and joints. The combination of severe pain, fatigue, and fever in this patient is more consistent with a vaso-occlusive crisis.
Correct Answer is D
Explanation
Choice A Reason:
Recommending cleaning the ear with cotton swabs daily is not appropriate for managing otitis externa. Using cotton swabs can further irritate the ear canal, potentially worsening the inflammation and increasing the risk of infection. It is generally advised to avoid inserting anything into the ear canal to prevent damage and irritation.
Choice B Reason:
Advising the patient to use over-the-counter ear drops is not the best initial intervention. While some over-the-counter ear drops may provide temporary relief, they are not as effective as prescription topical antibiotics and corticosteroids in treating the underlying infection and inflammation associated with otitis externa. Proper medical treatment is necessary to ensure effective management of the condition.
Choice C Reason:
Administering oral antibiotics is not typically the first-line treatment for uncomplicated otitis externa. Oral antibiotics are reserved for cases where the infection has spread beyond the ear canal or in patients with risk factors for severe infection. Topical antibiotics and corticosteroids are preferred for their direct action on the affected area and fewer systemic side effects.
Choice D Reason:
Administering topical antibiotics and corticosteroids is the most appropriate initial intervention for otitis externa. Topical treatments effectively target the infection and reduce inflammation, providing relief from symptoms such as pain, itching, and discharge. This approach is supported by clinical guidelines and is considered the standard of care for managing otitis externa.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
