Stroke: Ischemic stroke, Hemorrhagic stroke, Transient ischemic attack (TIA)
- The nervous system relies on a constant supply of oxygen and glucose from the blood to maintain its function and viability
- Ischemic stroke is a condition that occurs when the blood flow to a part of the brain is interrupted, resulting in tissue hypoxia, ischemia, and infarction
- The nervous system is highly sensitive to changes in blood flow, oxygen, glucose, and electrolytes, which can affect its function and structure.
- A stroke is a sudden interruption of blood flow to a part of the brain, resulting in tissue damage and neurological deficits.
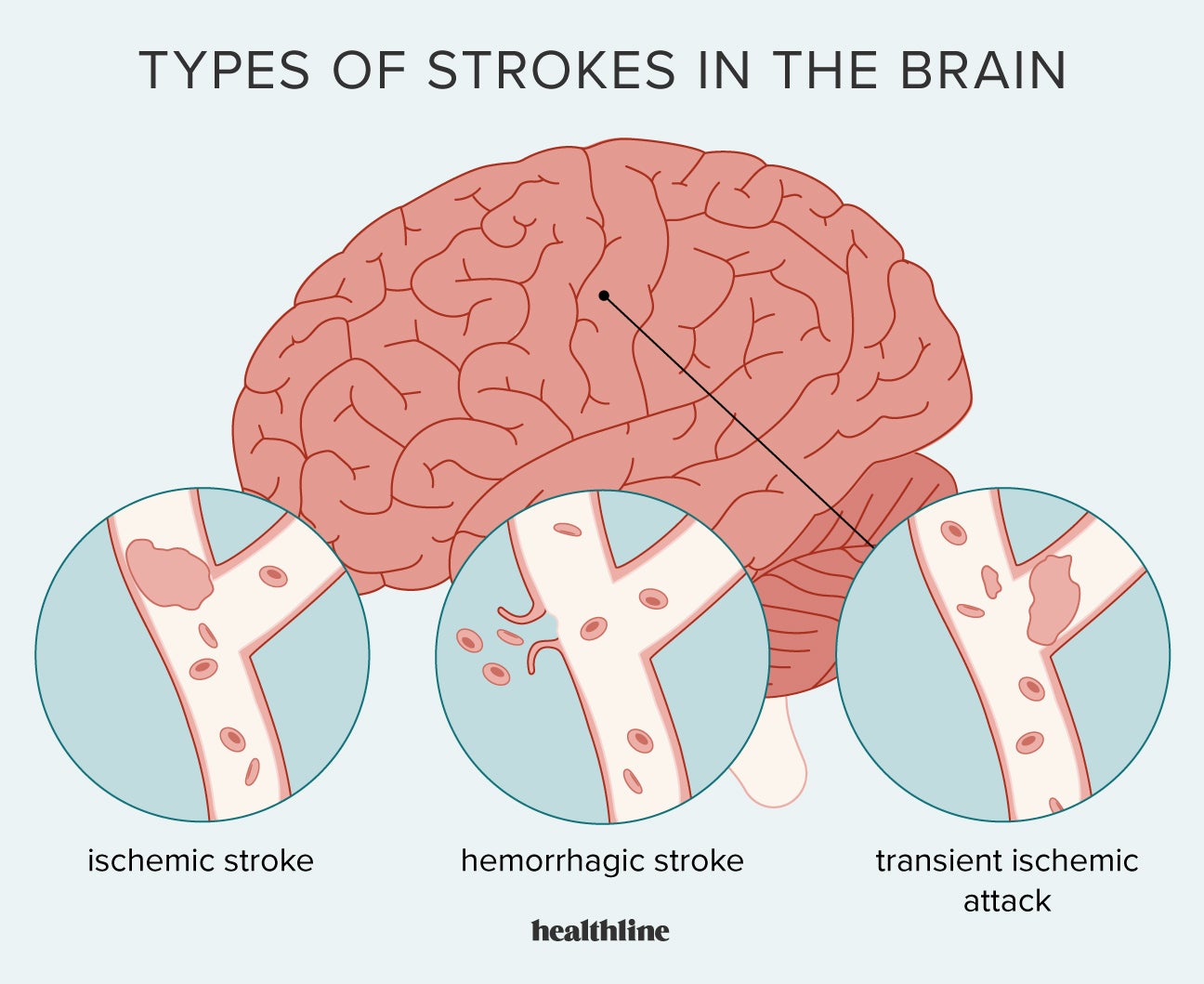
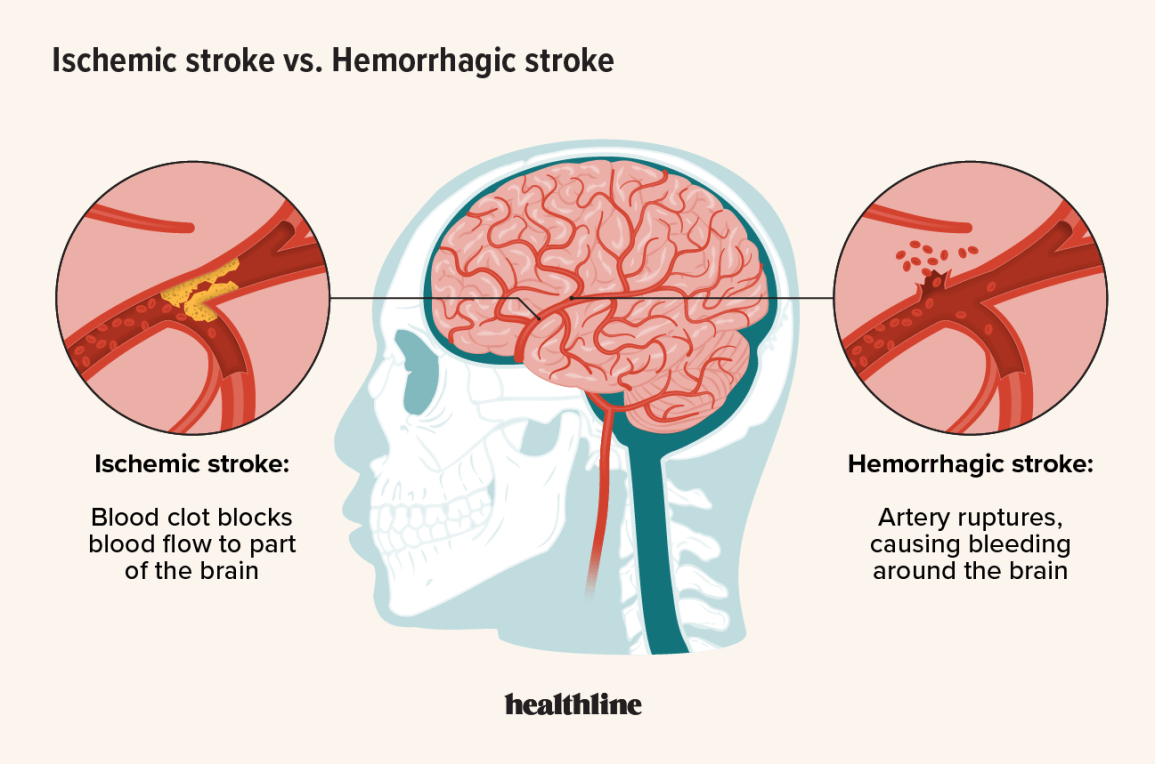
- A stroke can be classified as ischemic or hemorrhagic, depending on the underlying mechanism.
- Ischemic stroke is the most common type of stroke, accounting for about 80% of all strokes1
- Ischemic stroke can be classified into two main types: thrombotic and embolic2
- Thrombotic stroke occurs when a blood clot forms on an atherosclerotic plaque in a cerebral artery, blocking the blood flow to the downstream brain tissue
- Embolic stroke occurs when a blood clot or other debris travels from another part of the body (such as the heart or carotid artery) and lodges in a cerebral artery, cutting off the blood supply to the distal brain tissue
- Ischemic stroke can also be classified according to the location and size of the affected brain region3
- Large artery thrombotic stroke affects the major cerebral arteries, such as the internal carotid, middle cerebral, or anterior cerebral arteries
- Small penetrating artery thrombotic stroke affects the smaller branches of the cerebral arteries, such as the lenticulostriate arteries
- Cardiogenic embolic stroke affects any cerebral artery, depending on the source and size of the embolus
- Cryptogenic stroke is a term used when the cause of ischemic stroke is unknown or undetermined
- Other causes of ischemic stroke include vasculitis, dissection, hypercoagulable states, sickle cell disease, and cocaine abuse
- Ischemic stroke is associated with several modifiable and non-modifiable risk factors4
- Modifiable risk factors include hypertension, diabetes mellitus, dyslipidemia, smoking, obesity, physical inactivity, atrial fibrillation, coronary artery disease, carotid artery stenosis, oral contraceptive use, alcohol abuse, and illicit drug use
- Non-modifiable risk factors include age (increased risk after 55 years), sex (higher risk in men than women), race (higher risk in African Americans than Caucasians), family history, genetic factors, and low birth weight
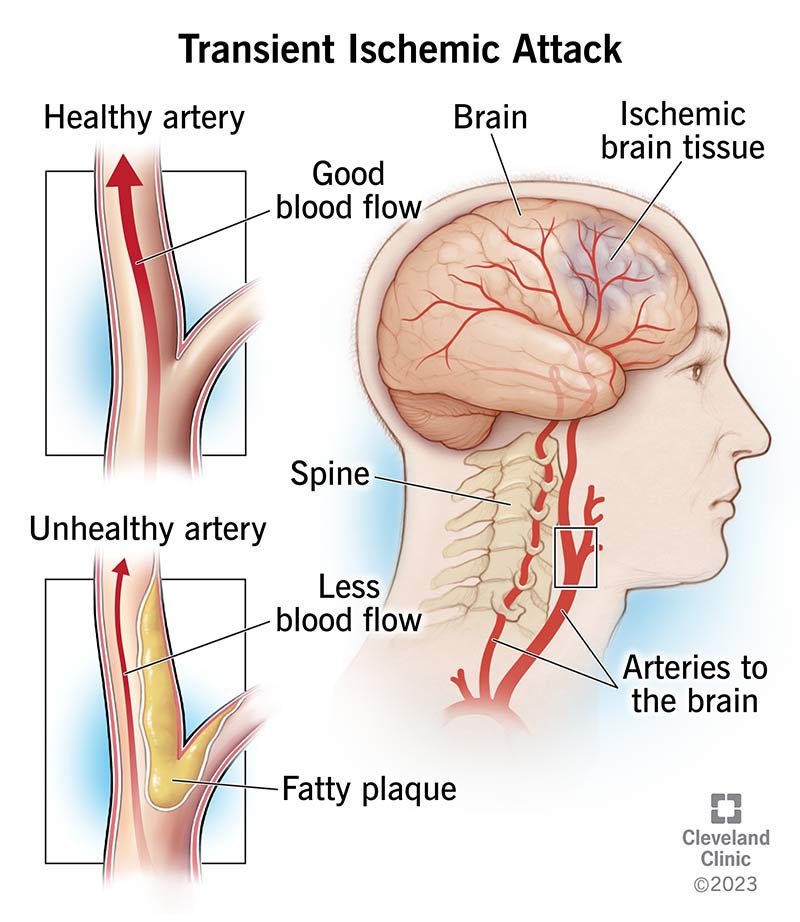
- The main cause of ischemic stroke is atherosclerosis, which is a chronic inflammatory process that leads to plaque formation and narrowing of the arterial lumen5
- Atherosclerosis can affect any artery in the body, but it is especially prevalent in the carotid and cerebral arteries
- Atherosclerosis can cause thrombotic stroke by inducing platelet aggregation and thrombus formation on the plaque surface
- Atherosclerosis can also cause embolic stroke by causing plaque rupture or ulceration, which can release fragments of plaque material or thrombus into the bloodstream
- Atherosclerosis can also reduce the collateral blood flow to the brain, making it more vulnerable to ischemia
- The pathophysiology of ischemic stroke involves a complex cascade of cellular and molecular events that lead to neuronal injury and death6
- When blood flow to a part of the brain is reduced below a critical threshold (about 25 ml/100 g/min), neurons switch from aerobic to anaerobic metabolism to produce ATP7
- Anaerobic metabolism is less efficient and produces lactic acid, which lowers the pH and causes acidosis
- Acidosis impairs the function of membrane pumps that maintain ionic gradients across neuronal membranes
- As a result, sodium and calcium ions accumulate inside neurons, while potassium ions leak out
- This leads to membrane depolarization, which triggers the release of excitatory neurotransmitters such as glutamate
- Glutamate binds to NMDA receptors on postsynaptic neurons, causing further influx of calcium and sodium ions
- Excess calcium activates various enzymes that degrade proteins, lipids, and DNA, leading to cell death by necrosis or apoptosis
- Excess glutamate also causes excitotoxicity, which damages neighboring neurons and glial cells
- The area of irreversible ischemic damage is called the infarct core, which is surrounded by a zone of potentially salvageable tissue called the ischemic penumbra
- The ischemic penumbra can be rescued by restoring blood flow within a narrow time window (about 3 to 4.5 hours), using thrombolytic therapy or mechanical thrombectomy
- The clinical manifestations of ischemic stroke depend on the location and extent of the brain injury8
- The most common symptoms of ischemic stroke are sudden onset of focal neurological deficits, such as weakness, numbness, visual loss, aphasia, dysarthria, dysphagia, ataxia, and vertigo
- The neurological deficits are usually contralateral to the side of the brain lesion, except for some cranial nerve deficits that are ipsilateral
- The neurological deficits can be assessed using the National Institutes of Health Stroke Scale (NIHSS), which is a standardized tool that evaluates 11 items related to level of consciousness, eye movements, visual fields, facial palsy, motor strength, limb ataxia, sensory loss, language, speech, and extinction9
- The NIHSS score ranges from 0 to 42, with higher scores indicating more severe stroke
- The neurological deficits can also be recognized using the FAST mnemonic, which stands for Face (ask the person to smile and check for facial droop), Arms (ask the person to raise both arms and check for arm drift), Speech (ask the person to repeat a simple sentence and check for slurred or inappropriate speech), and Time (note the time when symptoms started and call 911 immediately)10
- Some patients may also experience headache, nausea, vomiting, seizures, or altered mental status
- The diagnosis of ischemic stroke is based on clinical history, physical examination, and neuroimaging studies11
- Clinical history should include the onset, duration, and progression of symptoms, as well as the presence of risk factors and comorbidities
- Physical examination should include a comprehensive neurological assessment using the NIHSS or other validated scales
- Neuroimaging studies are essential to confirm the diagnosis of ischemic stroke, exclude hemorrhagic stroke or other causes of neurological deficits, identify the location and size of the brain lesion, and evaluate the vascular anatomy and perfusion status
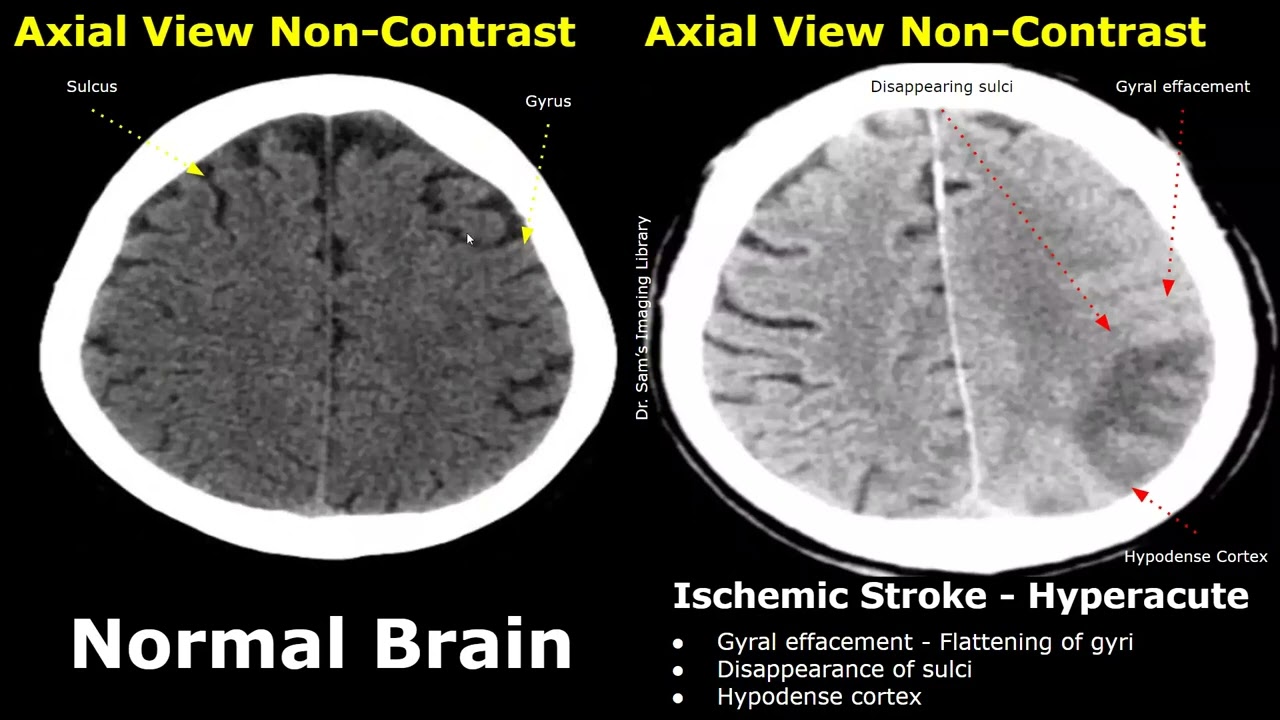
- The most commonly used neuroimaging modality for ischemic stroke is noncontrast computed tomography (CT) scan12
- CT scan is widely available, fast, and reliable in detecting intracranial hemorrhage
- CT scan can also show early signs of ischemic stroke in some cases, such as loss of gray-white matter differentiation, hypodensity in the affected brain region, or hyperdense artery sign
- CT scan can also be combined with CT angiography (CTA) or CT perfusion (CTP) to provide more information about the cerebral blood vessels and blood flow
- Another neuroimaging modality for ischemic stroke is magnetic resonance imaging (MRI)13
- MRI is more sensitive and specific than CT scan in detecting acute ischemic stroke, especially in the posterior fossa and subcortical regions
- MRI can also show different stages of ischemic stroke evolution using different sequences, such as diffusion-weighted imaging (DWI), perfusion-weighted imaging (PWI), fluid-attenuated inversion recovery (FLAIR), gradient-recalled echo (GRE), or susceptibility-weighted imaging (SWI)
- MRI can also be combined with magnetic resonance angiography (MRA) or magnetic resonance venography (MRV) to visualize the cerebral arteries and veins
- Other diagnostic tests and procedures for ischemic stroke include14
- Blood tests to measure glucose level, electrolytes, renal function, liver function, complete blood count, coagulation profile, lipid profile, cardiac enzymes, and inflammatory markers
- Electrocardiogram (ECG) to detect cardiac arrhythmias, ischemia, or infarction
- Echocardiogram to evaluate cardiac structure and function, and to detect potential sources of emboli, such as valvular disease, cardiac thrombi, or patent foramen ovale
- Carotid ultrasound to assess carotid artery stenosis or plaque morphology
- Transcranial Doppler to measure cerebral blood flow velocity and detect intracranial stenosis or emboli
- Ischemic stroke can lead to several complications that can worsen the prognosis and quality of life of patients
- Hemorrhagic transformation is a condition that occurs when blood leaks into the ischemic brain tissue, causing secondary hemorrhage and edema
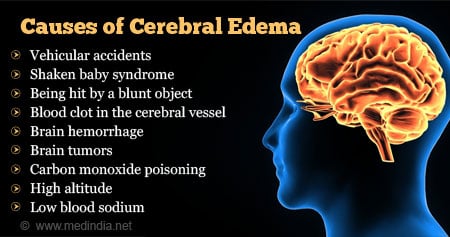
- Cerebral edema is a condition that occurs when fluid accumulates in the brain tissue, causing increased intracranial pressure and compression of vital structures
- Vasospasm is a condition that occurs when cerebral arteries constrict, reducing blood flow and causing delayed ischemia
- Seizures are abnormal electrical discharges in the brain that can cause convulsions, loss of consciousness, or other neurological symptoms
- Hydrocephalus is a condition that occurs when cerebrospinal fluid accumulates in the ventricles, causing increased intracranial pressure and impaired brain function
- Infections are conditions that occur when microorganisms invade the body, causing fever, inflammation, and systemic or local complications
- Dysphagia is a condition that occurs when swallowing muscles are impaired, causing difficulty or inability to swallow food, liquids, or saliva
- Aspiration pneumonia is a condition that occurs when food, liquids, or saliva enter the lungs, causing inflammation and infection
- Malnutrition is a condition that occurs when nutritional intake is inadequate, causing weight loss, muscle wasting, and impaired immunity
- Pressure ulcers are conditions that occur when skin and underlying tissues are damaged by prolonged pressure, friction, or shear forces
- Deep vein thrombosis (DVT) is a condition that occurs when blood clots form in the deep veins of the legs or pelvis, causing pain, swelling, and inflammation
- Pulmonary embolism (PE) is a condition that occurs when a blood clot from a DVT breaks off and travels to the lungs, causing chest pain, shortness of breath, and hypoxia
- Depression is a condition that occurs when mood is persistently low, causing sadness, hopelessness, loss of interest, and suicidal thoughts
- The therapeutic interventions for ischemic stroke aim to restore blood flow to the ischemic brain tissue, prevent further ischemia or hemorrhage, reduce complications, and improve functional recovery
- Thrombolytic therapy is a treatment that involves administering an intravenous drug (such as alteplase) that dissolves the blood clot and restores blood flow to the affected brain region
- Thrombolytic therapy can reduce the disability and mortality from ischemic stroke if given within 4.5 hours of symptom onset
- Thrombolytic therapy has several contraindications and risks, such as hemorrhagic stroke, intracranial hemorrhage, or systemic bleeding
- Thrombolytic therapy requires careful monitoring of vital signs, neurological status, and coagulation parameters
- Mechanical thrombectomy is a treatment that involves inserting a catheter through a groin artery and advancing it to the occluded cerebral artery, where a device (such as a stent retriever or an aspiration catheter) is used to remove the clot and restore blood flow
- Mechanical thrombectomy can improve the outcomes of ischemic stroke if performed within 6 hours of symptom onset, or up to 24 hours in selected cases
- Mechanical thrombectomy has some limitations and complications, such as difficulty in accessing the clot, vessel perforation, or distal embolization
- Mechanical thrombectomy requires specialized equipment and personnel, and close collaboration between neurologists, radiologists, and neurosurgeons
- Anticoagulant therapy is a treatment that involves administering drugs (such as heparin or warfarin) that prevent the formation or extension of blood clots
- Anticoagulant therapy can prevent recurrent ischemic stroke in patients with atrial fibrillation or other cardiac sources of emboli
- Anticoagulant therapy has several contraindications and risks, such as hemorrhagic stroke, intracranial hemorrhage, or systemic bleeding
- Anticoagulant therapy requires regular monitoring of coagulation parameters (such as INR) and adjustment of drug dosage
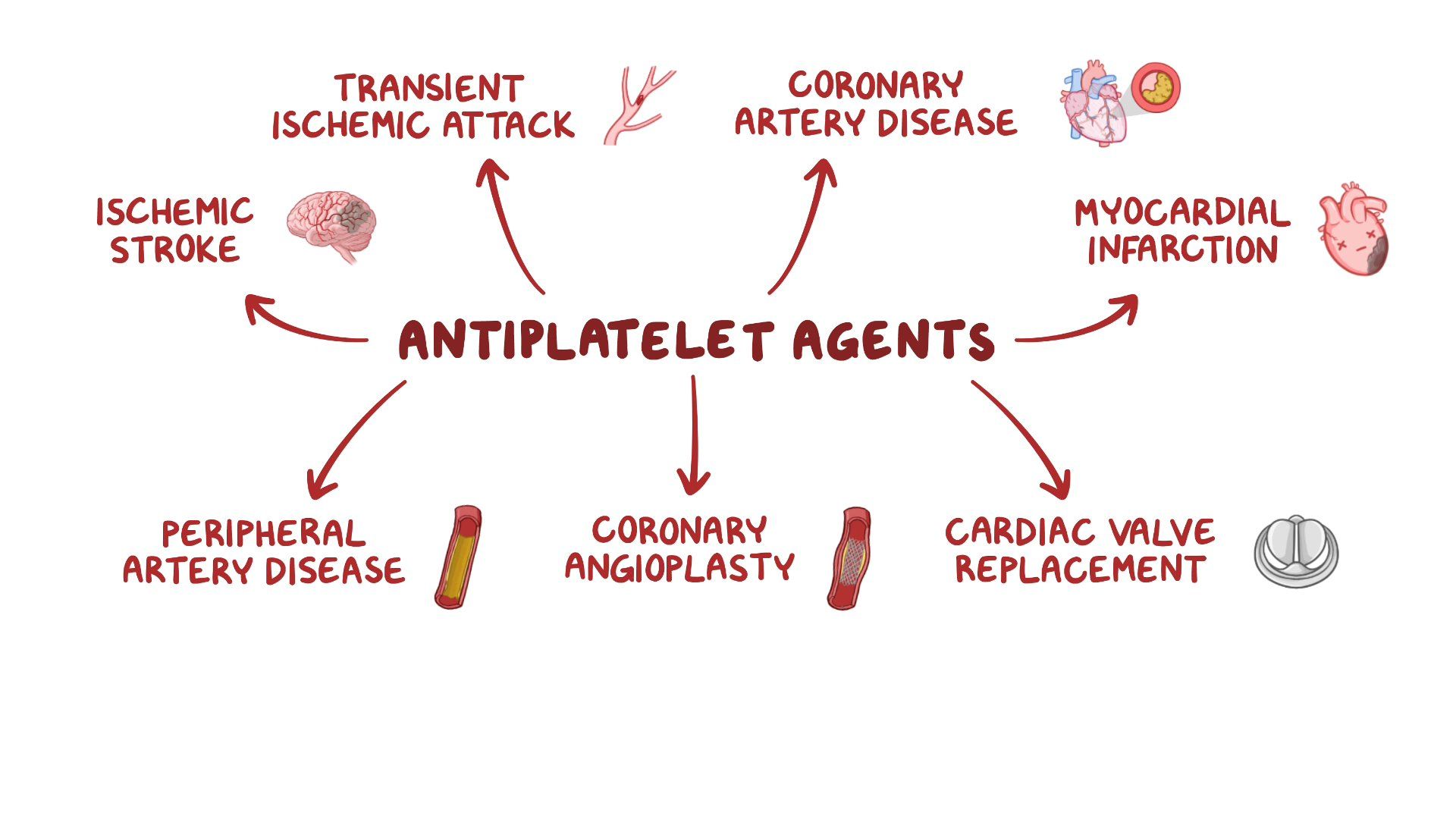
- Antiplatelet therapy is a treatment that involves administering drugs (such as aspirin or clopidogrel) that inhibit platelet aggregation and adhesion
- Antiplatelet therapy can prevent recurrent ischemic stroke in patients with noncardioembolic stroke or transient ischemic attack (TIA)
- Antiplatelet therapy has some contraindications and risks, such as hemorrhagic stroke, intracranial hemorrhage, or gastrointestinal bleeding
- Antiplatelet therapy does not require routine monitoring of coagulation parameters, but may interact with other drugs or foods
- Neuroprotective therapy is a treatment that involves administering drugs (such as magnesium or nimodipine) that protect the brain cells from ischemic injury by modulating calcium influx, glutamate release, or oxidative stress
- Neuroprotective therapy has shown promising results in animal models of ischemic stroke, but has failed to demonstrate efficacy in human trials
- Neuroprotective therapy has some adverse effects, such as hypotension, bradycardia, or headache
- Neuroprotective therapy is still under investigation and not widely used in clinical practice
- Surgical intervention is a treatment that involves performing a procedure (such as carotid endarterectomy, carotid stenting, or decompressive craniectomy) that removes the source of ischemia or reduces the intracranial pressure
- Surgical intervention can prevent recurrent ischemic stroke in patients with severe carotid artery stenosis or symptomatic intracranial stenosis
- Surgical intervention can also improve the survival and outcome of patients with malignant cerebral edema or large hemispheric infarction
- Surgical intervention has some indications and risks, such as perioperative stroke, infection, or bleeding
- Surgical intervention requires careful selection of candidates and timing of surgery, and multidisciplinary collaboration between neurologists, vascular surgeons, and neurosurgeons
- Rehabilitation is a treatment that involves providing physical, occupational, speech, and psychological therapies that aim to restore function, independence, and quality of life of patients with ischemic stroke
- Rehabilitation can improve the motor, sensory, cognitive, linguistic, and emotional recovery of patients with ischemic stroke
- Rehabilitation can also prevent complications such as contractures, spasticity, falls, infections, depression, or social isolation
- Rehabilitation requires a comprehensive assessment of the patient’s needs and goals, and a tailored plan of interventions that involve the patient, family, and caregivers
- Rehabilitation should start as soon as possible after ischemic stroke and continue for as long as needed
- Thrombolytic therapy is a treatment that involves administering an intravenous drug (such as alteplase) that dissolves the blood clot and restores blood flow to the affected brain region
- Nursing care for patients with ischemic stroke involves providing holistic and evidence-based care that addresses the physical, psychological, and social needs of the patient and family
- Nursing care should follow the nursing process of assessment, diagnosis, planning, implementation, and evaluation
- Nursing care should be based on the best available research and guidelines, such as the American Stroke Association (ASA) guidelines or the Stroke Best Practice Recommendations (SBPR)
- Nursing care should be delivered by a competent and compassionate nurse who works as part of an interdisciplinary stroke team
- Nursing assessment for patients with ischemic stroke involves collecting subjective and objective data that are relevant to the patient’s condition and response to treatment
- Subjective data include the patient’s history of present illness, past medical history, family history, medication history, allergy history, social history, and review of systems
- Objective data include the patient’s vital signs, neurological examination using the NIHSS or other scales, cardiovascular examination using the ECG or echocardiogram, vascular examination using the carotid ultrasound or transcranial Doppler, laboratory tests such as blood glucose level or coagulation profile, and neuroimaging studies such as CT scan or MRI
- Nursing diagnosis for patients with ischemic stroke involves identifying the actual or potential problems that affect the patient’s health and well-being
- Some examples of nursing diagnoses for patients with ischemic stroke are:
- Ineffective tissue perfusion related to reduced cerebral blood flow
- Impaired physical mobility related to hemiparesis or hemiplegia
- Impaired verbal communication related to aphasia or dysarthria
- Impaired swallowing related to dysphagia or cranial nerve deficits
- Risk for aspiration related to impaired swallowing or decreased level of consciousness
- Risk for infection related to impaired immunity or invasive procedures
- Risk for injury related to seizures or falls
- Risk for impaired skin integrity related to immobility or pressure ulcers
- Risk for venous thromboembolism related to immobility or hypercoagulability
- Acute pain related to headache or muscle spasms
- Anxiety related to fear of death or disability
- Depression related to loss of function or social support
- Some examples of nursing diagnoses for patients with ischemic stroke are:
- Nursing planning for patients with ischemic stroke involves setting realistic and measurable goals and outcomes that are based on the patient’s needs, preferences, and potential
- Some examples of nursing goals and outcomes for patients with ischemic stroke are:
- The patient will maintain adequate tissue perfusion as evidenced by normal vital signs, neurological status, and neuroimaging findings
- The patient will improve physical mobility as evidenced by increased range of motion, strength, and coordination of the affected limbs
- The patient will improve verbal communication as evidenced by increased comprehension, expression, and articulation of speech
- The patient will improve swallowing as evidenced by decreased risk of aspiration, improved oral intake, and normal weight
- The patient will prevent infection as evidenced by absence of fever, inflammation, or positive cultures
- The patient will prevent injury as evidenced by absence of seizures, falls, or trauma
- The patient will prevent impaired skin integrity as evidenced by absence of pressure ulcers, erythema, or breakdown
- The patient will prevent venous thromboembolism as evidenced by absence of pain, swelling, or inflammation in the lower extremities or chest
- The patient will manage pain as evidenced by decreased pain intensity, frequency, and duration
- The patient will reduce anxiety as evidenced by decreased heart rate, blood pressure, and respiratory rate
- The patient will cope with depression as evidenced by increased mood, interest, and social interaction
- Some examples of nursing goals and outcomes for patients with ischemic stroke are:
- Nursing implementation for patients with ischemic stroke involves performing interventions that are consistent with the nursing diagnoses, goals, and outcomes
- Some examples of nursing interventions for patients with ischemic stroke are:
- Monitor vital signs, neurological status, and coagulation parameters frequently and report any changes or abnormalities to the physician
- Administer thrombolytic therapy, anticoagulant therapy, antiplatelet therapy, or neuroprotective therapy as prescribed and monitor for any adverse effects or complications
- Assist with mechanical thrombectomy or surgical intervention as needed and monitor for any perioperative or postoperative complications
- Maintain a patent airway and oxygen saturation above 95% by providing supplemental oxygen, suctioning, or intubation as needed
- Elevate the head of the bed to 30 degrees and position the patient on the unaffected side to reduce intracranial pressure and facilitate drainage
- Assess swallowing function using a bedside swallow test or a videofluoroscopic swallow study and provide appropriate oral care and hydration
- Initiate enteral or parenteral nutrition as prescribed and monitor for any signs of intolerance or malabsorption
- Prevent aspiration pneumonia by elevating the head of the bed to 45 degrees during feeding, thickening liquids, using chin tuck or swallow maneuvers, and administering prophylactic antibiotics as prescribed
- Encourage early mobilization and exercise of the affected limbs using passive, active, or resistive movements, and provide assistive devices such as braces, splints, or walkers as needed
- Some examples of nursing interventions for patients with ischemic stroke are:
- Prevent contractures and spasticity by applying range of motion exercises, heat, cold, or massage therapy, and administering muscle relaxants or botulinum toxin injections as prescribed
- Prevent pressure ulcers by repositioning the patient every 2 hours, using pressure-relieving mattresses or cushions, and inspecting the skin for any signs of breakdown or infection
- Prevent venous thromboembolism by applying compression stockings or pneumatic devices, elevating the lower extremities, and administering anticoagulants or thrombolytics as prescribed
- Manage pain by assessing its location, intensity, and quality using a valid scale (such as the numeric rating scale or the faces pain scale), and administering analgesics or nonpharmacological methods (such as relaxation techniques or distraction) as prescribed
- Reduce anxiety by providing reassurance, information, and emotional support to the patient and family, and administering anxiolytics or sedatives as prescribed
- Cope with depression by assessing its severity using a valid tool (such as the Hamilton depression rating scale or the Beck depression inventory), and administering antidepressants or psychotherapy as prescribed
- Improve verbal communication by assessing the type and severity of aphasia using a valid tool (such as the Boston diagnostic aphasia examination or the Western aphasia battery), and providing speech therapy or augmentative communication devices (such as picture boards or computer programs) as needed
- Promote cognitive function by assessing the presence and extent of cognitive impairment using a valid tool (such as the mini-mental state examination or the Montreal cognitive assessment), and providing cognitive stimulation or rehabilitation activities (such as memory games or puzzles) as needed
- Facilitate social interaction by encouraging family and friends to visit and participate in care, and providing opportunities for group activities or support groups as available
- Nursing evaluation for patients with ischemic stroke involves measuring the effectiveness of the interventions and comparing them with the expected outcomes
- Nursing evaluation should be done continuously and systematically throughout the care process
- Nursing evaluation should involve the patient, family, and other members of the stroke team
- Nursing evaluation should use the same tools and scales that were used for the assessment and planning phases
- Nursing evaluation should document the results and findings in a clear and concise manner
- Nursing evaluation should identify any gaps or discrepancies between the actual and expected outcomes
- Nursing evaluation should modify or revise the nursing diagnoses, goals, outcomes, or interventions as needed
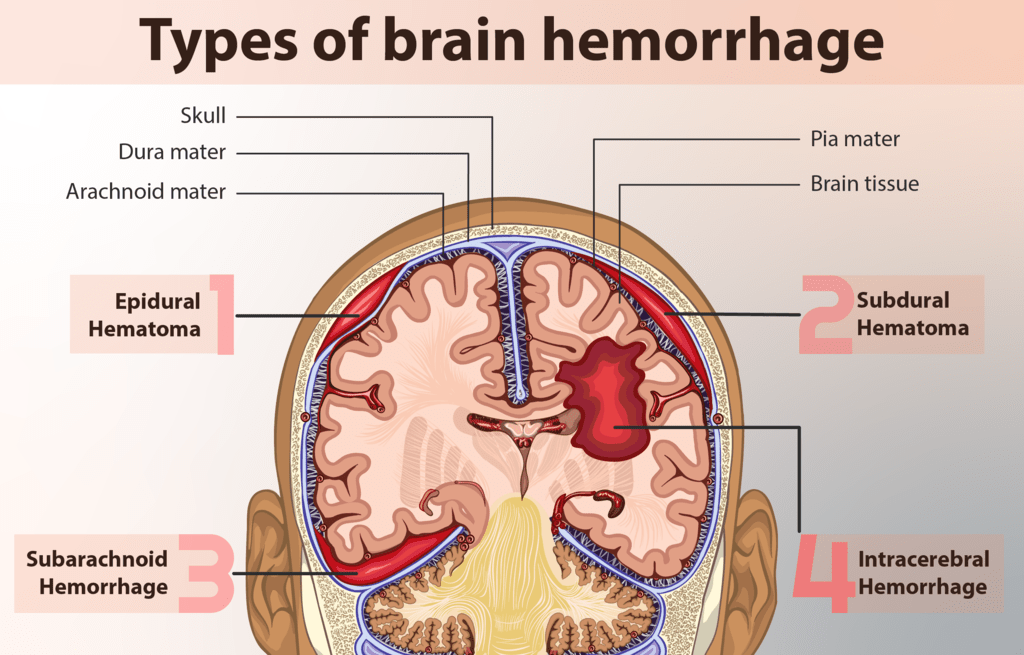
- A hemorrhagic stroke occurs when a blood vessel in the brain ruptures and bleeds into the surrounding brain tissue or into the subarachnoid space (the space between the brain and the meninges).
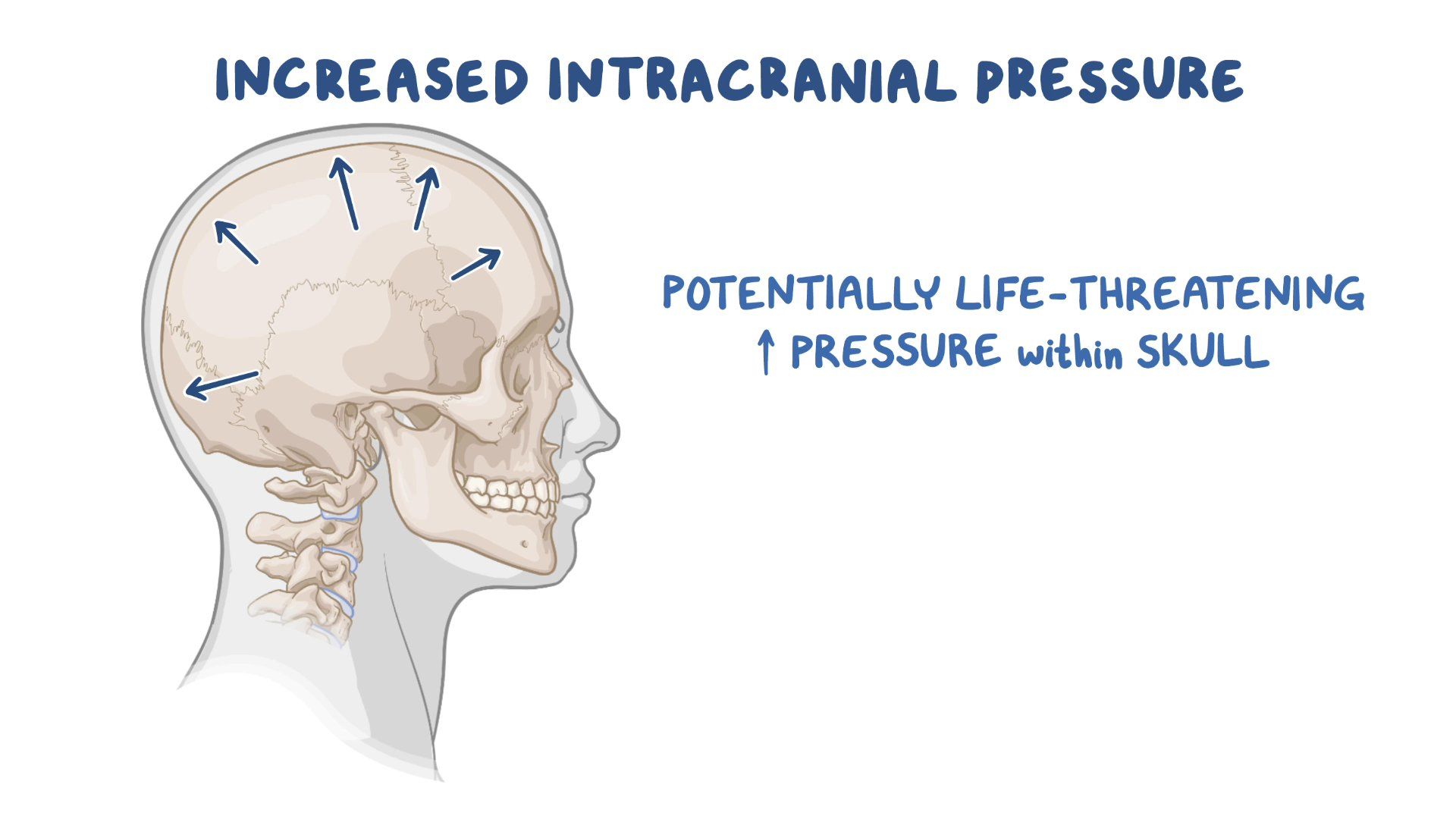
- The bleeding causes increased intracranial pressure (ICP), which compresses and damages the brain tissue, as well as reduces cerebral perfusion pressure (CPP), which impairs blood flow to the brain.
- A hemorrhagic stroke can be further classified as intracerebral or subarachnoid, depending on the location of the bleeding.
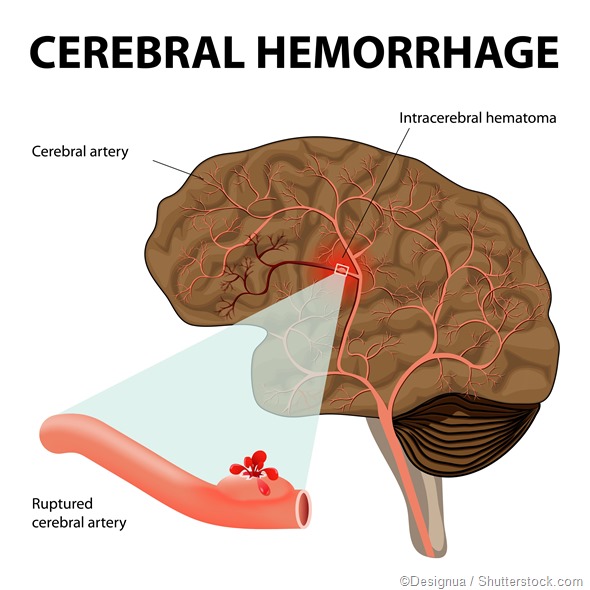
- An intracerebral hemorrhage (ICH) is a type of hemorrhagic stroke that occurs when a blood vessel within the brain parenchyma (the functional tissue) ruptures and bleeds into the brain tissue.
- The most common cause of ICH is hypertension, which weakens the walls of small arteries in the brain over time. Other causes include trauma, vascular malformations, tumors, coagulopathy, amyloid angiopathy, and illicit drug use.
- The signs and symptoms of ICH depend on the location and extent of bleeding, but may include headache, nausea, vomiting, altered level of consciousness, hemiparesis (weakness on one side of the body), hemiplegia (paralysis on one side of the body), aphasia (language impairment), dysarthria (speech impairment), dysphagia (swallowing impairment), ataxia (coordination impairment), visual disturbances, seizures, and coma.
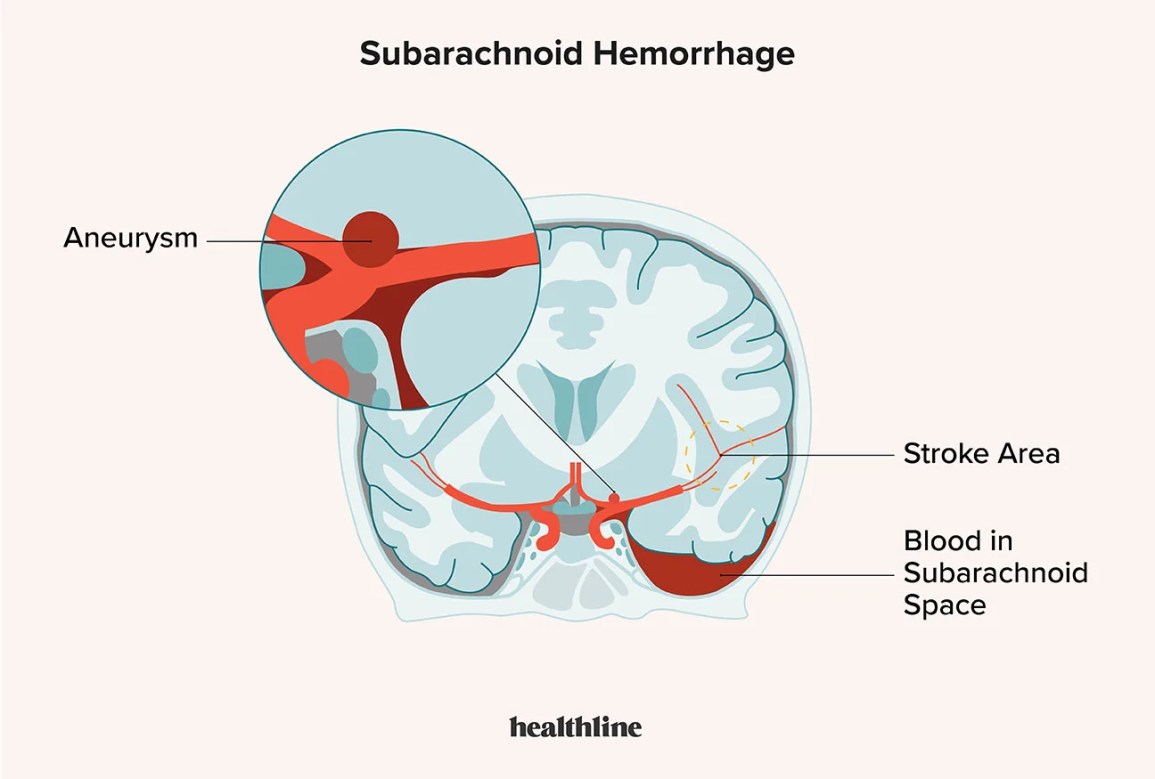
- A subarachnoid hemorrhage (SAH) is a type of hemorrhagic stroke that occurs when a blood vessel between the brain and the meninges ruptures and bleeds into the subarachnoid space.
- The most common cause of SAH is a ruptured cerebral aneurysm, which is a bulging or ballooning of a weakened area in an artery wall. Other causes include trauma, vascular malformations, tumors, coagulopathy, and illicit drug use.
- The signs and symptoms of SAH include sudden severe headache ("thunderclap headache"), nausea, vomiting, neck stiffness ("nuchal rigidity"), photophobia (sensitivity to light), altered level of consciousness, focal neurological deficits (such as hemiparesis or aphasia), cranial nerve palsies (such as ptosis or diplopia), seizures, and coma.
- The diagnosis of hemorrhagic stroke is based on clinical presentation, medical history, physical examination, neurological assessment, and imaging studies.
- The imaging studies that are used to confirm hemorrhagic stroke are computed tomography (CT) scan or magnetic resonance imaging (MRI) scan of the head. These tests can show the location and extent of bleeding in the brain. They can also help differentiate between ischemic and hemorrhagic stroke.
- Other tests that may be performed to identify the cause or complications of hemorrhagic stroke include lumbar puncture (to obtain cerebrospinal fluid for analysis), angiography (to visualize blood vessels in the brain), electroencephalography (to monitor brain activity), blood tests (to check for coagulation disorders or infection), chest X-ray (to rule out cardiac or pulmonary sources of emboli), electrocardiogram (to assess cardiac function), echocardiogram (to evaluate cardiac structure and function), carotid ultrasound (to assess carotid artery stenosis or plaque).
- The treatment of hemorrhagic stroke aims to stop bleeding, reduce ICP, prevent complications, and restore neurological function.
- The treatment options depend on the type, location, and severity of bleeding, as well as the patient's condition and preferences.
- The treatment options may include medical management, surgical intervention, or endovascular therapy.
-
- Medical Management
- Medical management of hemorrhagic stroke involves supportive care and pharmacological therapy.
- Supportive care includes monitoring vital signs, neurological status, ICP, CPP, fluid and electrolyte balance, oxygenation, and glucose levels. It also includes maintaining a patent airway, providing adequate ventilation, ensuring proper positioning and alignment, preventing aspiration and infection, managing pain and fever, and providing nutritional support.
- Pharmacological therapy includes administering medications to control blood pressure, reduce ICP, prevent seizures, prevent vasospasm (narrowing of blood vessels), prevent or treat coagulopathy or infection, and provide sedation or analgesia.
- Surgical Intervention
- Surgical intervention of hemorrhagic stroke involves removing the source of bleeding or decompressing the brain tissue.
- The surgical procedures that may be performed include craniotomy (opening the skull to access the brain), hematoma evacuation (removing the blood clot from the brain), aneurysm clipping (placing a metal clip on the neck of the aneurysm to stop blood flow), ventriculostomy (inserting a catheter into a ventricle to drain excess cerebrospinal fluid and reduce ICP), or craniectomy (removing a part of the skull to allow brain swelling).
- Endovascular Therapy
- Endovascular therapy of hemorrhagic stroke involves using catheters and devices to treat the blood vessel abnormalities that cause bleeding.
- The endovascular procedures that may be performed include aneurysm coiling (placing coils into the aneurysm to block blood flow and induce clotting), aneurysm stenting (placing a stent into the artery to support the vessel wall and prevent rebleeding), or embolization (injecting glue or particles into the vessel to occlude it).
- Medical Management
- The prevention of hemorrhagic stroke involves identifying and modifying risk factors, screening for vascular abnormalities, and taking prophylactic medications.
- The risk factors for hemorrhagic stroke include hypertension, smoking, alcohol abuse, obesity, diabetes mellitus, hyperlipidemia, atrial fibrillation, oral contraceptive use, anticoagulant use, illicit drug use, family history of stroke or aneurysm, and age.
- The screening for vascular abnormalities includes performing imaging studies such as CT scan, MRI scan, or angiography to detect aneurysms or malformations in asymptomatic patients who have a high risk of bleeding.
- The prophylactic medications include taking antihypertensive drugs to control blood pressure, antiplatelet drugs to prevent thrombosis in patients with ischemic stroke or transient ischemic attack (TIA), statins to lower cholesterol levels, and anticonvulsants to prevent seizures in patients with SAH.
- The nursing interventions for hemorrhagic stroke are based on the nursing process: assessment, diagnosis, planning, implementation, and evaluation.
- Assessment: The nurse should assess the patient's vital signs, neurological status (using tools such as Glasgow Coma Scale or NIH Stroke Scale), ICP and CPP (if monitored), oxygenation and ventilation (using pulse oximetry or arterial blood gas analysis), fluid and electrolyte balance (using intake and output measurement or laboratory tests), pain level (using scales such as Numeric Rating Scale or Wong-Baker Faces Scale), skin integrity (using tools such as Braden Scale or Norton Scale), nutritional status (using tools such as Body Mass Index or Albumin Level), bowel and bladder function (using tools such as Bristol Stool Chart or Urine Color Chart), psychosocial status (using tools such as Beck Depression Inventory or Hamilton Anxiety Rating Scale), and family support and coping skills.
- Diagnosis: The nurse should identify the patient's actual or potential problems related to hemorrhagic stroke.
- Some examples of nursing diagnoses are: Ineffective tissue perfusion related to bleeding in the brain;
- Increased intracranial pressure related to hematoma formation; Impaired physical mobility related to hemiparesis or hemiplegia;
- Impaired verbal communication related to aphasia or dysarthria; Impaired swallowing related to dysphagia; Risk for aspiration related to impaired cough reflex;
- Risk for infection related to invasive procedures or immunosuppression; Acute pain related to increased ICP or surgical incision; Anxiety related to fear of death or disability;
- Powerlessness related to loss of control or independence; Deficient knowledge related to disease process or treatment regimen.
- Planning: The nurse should establish goals and expected outcomes for the patient based on the nursing diagnoses.
- Some examples of goals are: The patient will maintain adequate tissue perfusion as evidenced by normal vital signs, neurological status, ICP, CPP, oxygenation, and glucose levels;
- The patient will demonstrate improved physical mobility as evidenced by increased range of motion, strength, and coordination;
- The patient will express understanding of verbal and nonverbal messages as evidenced by appropriate responses and feedback; The patient will swallow safely and effectively as evidenced by absence of coughing, choking, or aspiration;
- The patient will remain free from infection as evidenced by normal temperature, white blood cell count, and wound healing;
- The patient will report pain relief as evidenced by decreased pain score and increased comfort level; The patient will exhibit reduced anxiety as evidenced by relaxed demeanor, positive coping strategies, and verbalization of feelings;
- The patient will demonstrate knowledge of disease process and treatment regimen as evidenced by verbalization, return demonstration, or written materials.
- Implementation: The nurse should perform the interventions that are appropriate for the patient's condition and goals.
- Some examples of interventions are:
- Administer medications as prescribed to control blood pressure,
- reduce ICP,
- prevent seizures,
- prevent vasospasm,
- prevent or treat coagulopathy or infection,
- and provide sedation or analgesia;
- Monitor vital signs, neurological status, ICP, CPP, oxygenation, ventilation, fluid and electrolyte balance, glucose levels, pain level, skin integrity, nutritional status, bowel and bladder function, psychosocial status, and family support and coping skills;
- Maintain a patent airway, provide adequate ventilation, suction secretions as needed, and administer oxygen therapy as ordered;
- Ensure proper positioning and alignment of the patient, elevate the head of the bed to 30 degrees or as ordered, avoid extreme flexion or rotation of the neck, and prevent valsalva maneuver;
- Prevent aspiration and infection by performing oral hygiene, providing thickened liquids or pureed foods as indicated, using a nasogastric tube or a percutaneous endoscopic gastrostomy (PEG) tube for enteral feeding if necessary, and using sterile technique for invasive procedures;
- Promote physical mobility by performing passive or active range of motion exercises, applying splints or braces as needed, assisting with transfers and ambulation as tolerated, and providing assistive devices such as a cane or a walker if indicated;
- Enhance verbal communication by using simple and clear language, speaking slowly and loudly, allowing time for the patient to respond, using gestures or pictures to supplement verbal messages, and providing alternative methods of communication such as a pen and paper or an electronic device if needed;
- Improve swallowing by assessing the patient's gag reflex and swallow function before each feeding, placing the patient in an upright position during and after feeding, offering small bites and sips of food and liquid at a time, instructing the patient to tuck the chin down when swallowing, and observing for signs of aspiration such as coughing, choking, or wheezing; Educate the patient and family about the disease process and treatment regimen,
- A TIA occurs when a blood clot or a piece of plaque blocks or narrows an artery that supplies blood to a part of the brain. The blockage is usually temporary and resolves within 24 hours, often within minutes or hours.
- The nervous system has three main functions: sensory, integrative, and motor
- Ischemia is reduced or interrupted blood flow to a part of the brain
- Hypoxia and anoxia are low or no oxygen levels in the affected brain tissue
- TIA is a temporary episode of neurological dysfunction caused by focal ischemia without infarction
- TIA is also known as a mini-stroke or a warning stroke
- TIA can indicate a high risk of a future stroke
- Stroke is a more severe form of ischemia that results in infarction and irreversible damage to the brain tissue
- There are two main types of stroke: ischemic stroke and hemorrhagic stroke
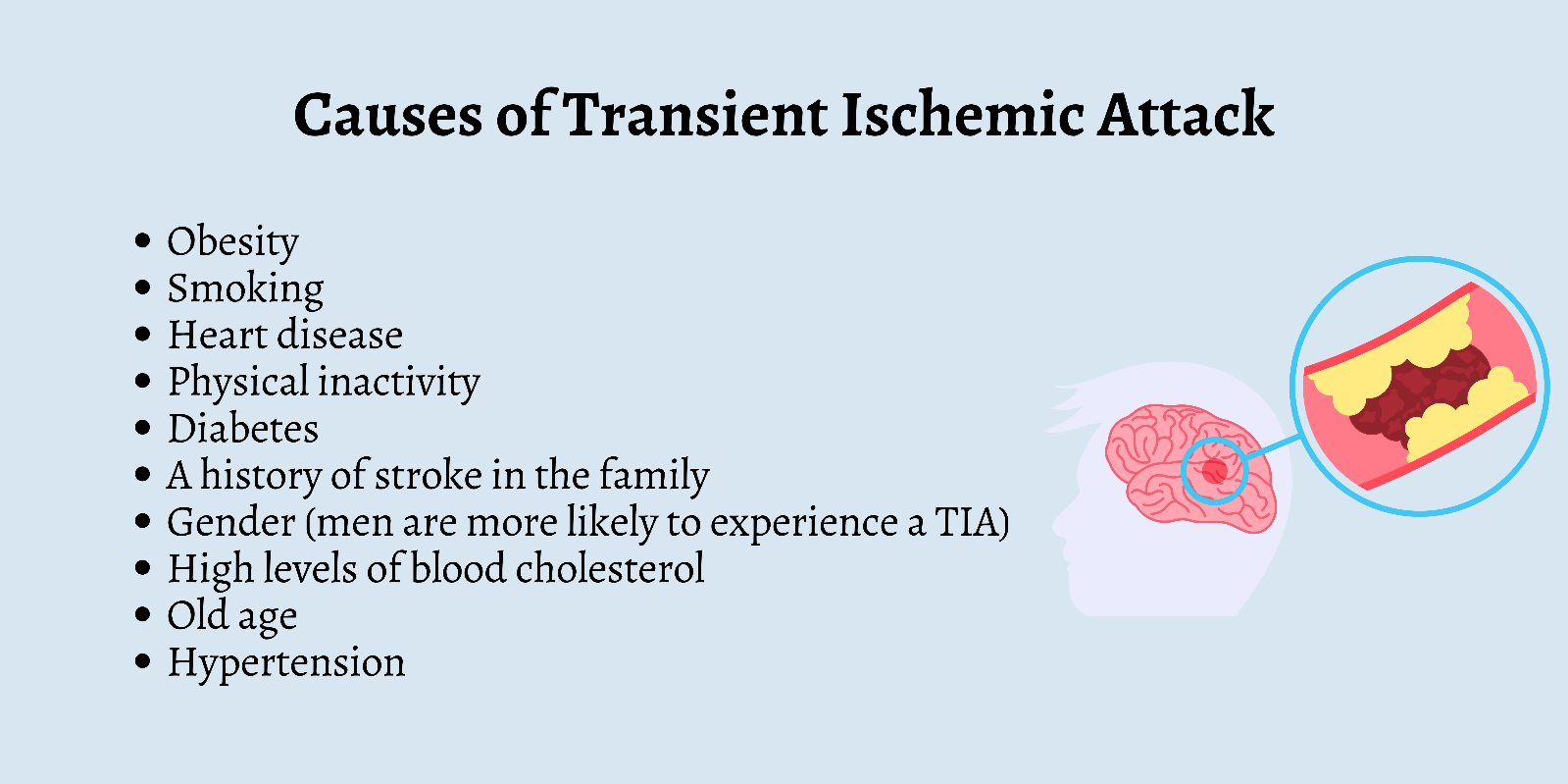
- The risk factors for TIA and ischemic stroke are similar
- The diagnosis of TIA is based on clinical observation, assessment of risk factors, and neuroimaging tests
- The management of TIA aims to prevent a future stroke by restoring blood flow, reducing modifiable risk factors, and using antiplatelet or anticoagulant medications
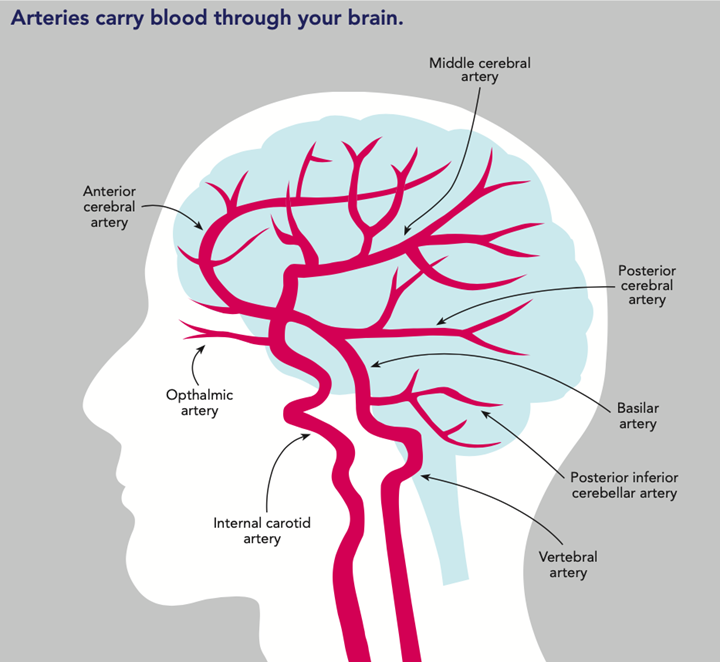
- The main arteries that supply blood to the brain are the internal carotid arteries and the vertebral arteries
- The internal carotid arteries branch into the anterior cerebral arteries and the middle cerebral arteries
- The vertebral arteries join to form the basilar artery, which branches into the posterior cerebral arteries
- The anterior, middle, and posterior cerebral arteries supply blood to different regions of the brain with different functions
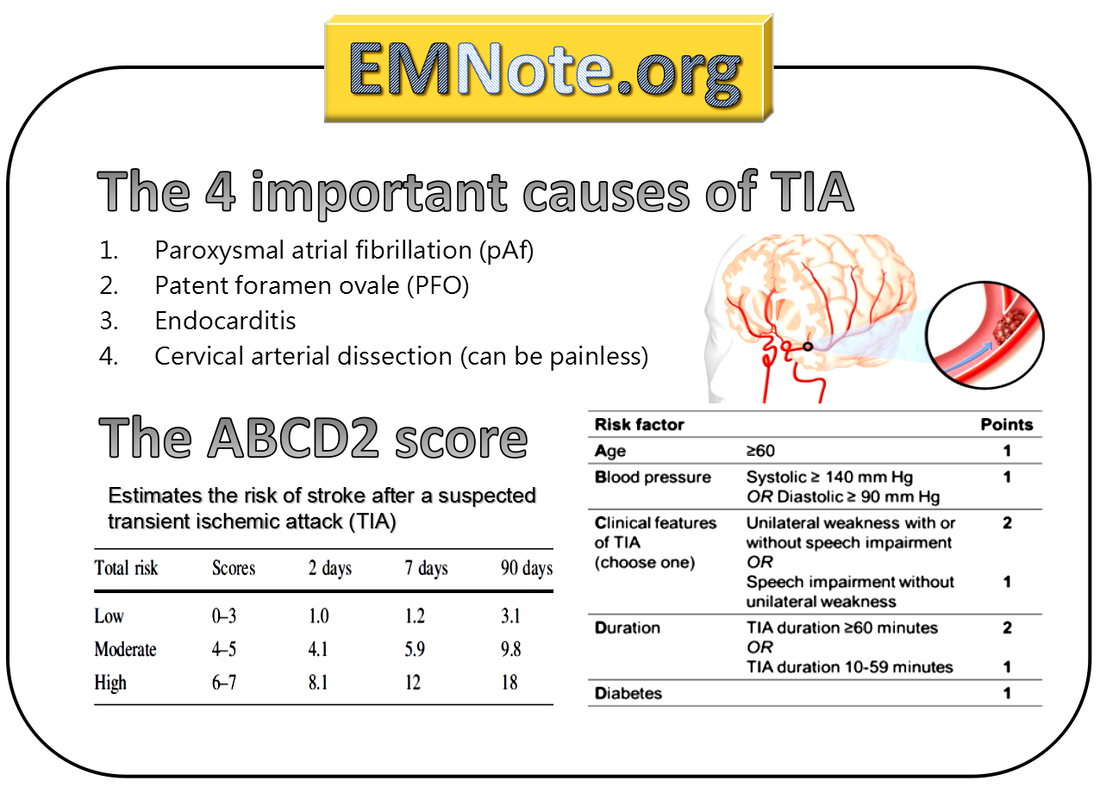
- The ABCD2 score is a tool designed to predict the risk of stroke in the 3-90 days after a TIA
- The ABCD2 score is based on five factors: age, blood pressure, clinical features, duration of symptoms, and diabetes
- The ABCD2 score can help clinicians decide whether to admit a patient with TIA to the hospital or to manage them as an outpatient
- The symptoms of a TIA depend on which artery is affected and which region of the brain is deprived of blood. The symptoms may include:
- Weakness or numbness in one side of the face, arm, or leg
- Difficulty speaking or understanding speech
- Loss or blurring of vision in one or both eyes
- Dizziness, vertigo, or loss of balance
- Severe headache with no known cause
- The symptoms of a TIA are similar to those of an ischemic stroke, but they are reversible and do not cause permanent damage to the brain. However, a TIA is a serious medical emergency that requires immediate attention, because it can be a sign of an impending stroke.
- A stroke is a more severe form of ischemia that results in infarction and irreversible damage to the brain tissue.
- A stroke can cause lasting disability or death.
- There are two main types of stroke: ischemic stroke and hemorrhagic stroke.
- An ischemic stroke occurs when a blood clot or a piece of plaque blocks an artery that supplies blood to a part of the brain, causing infarction.
- A hemorrhagic stroke occurs when an artery in or around the brain ruptures, causing bleeding into the brain tissue or the surrounding space.
- Age (older than 60 years)
- Hypertension (high blood pressure)
- Diabetes mellitus
- Hyperlipidemia (high cholesterol)
- Atrial fibrillation (irregular heartbeat)
- Smoking
- Obesity
- Physical inactivity
- Family history of stroke
- Previous history of TIA or stroke
- The diagnosis of TIA is based on clinical observation of signs and symptoms, assessment of risk factors, and neuroimaging tests.
- The neuroimaging tests include computed tomography (CT) scan or magnetic resonance imaging (MRI) scan of the brain to rule out hemorrhage or infarction.
- Other tests may include carotid ultrasound, echocardiogram, electrocardiogram (EKG), blood tests, and angiography.
- The management of TIA aims to prevent a future stroke by restoring blood flow to the affected area, reducing modifiable risk factors, and using antiplatelet or anticoagulant medications.
- Antiplatelet medications such as aspirin prevent platelets from sticking together and forming clots.
- Anticoagulant medications such as warfarin prevent blood from clotting.
- Some patients may also benefit from surgical procedures such as carotid endarterectomy or stenting to remove or widen a narrowed artery.
- The brain receives blood from two pairs of arteries: the internal carotid arteries and the vertebral arteries.
- The internal carotid arteries branch into the anterior cerebral arteries and the middle cerebral arteries.
- The vertebral arteries join to form the basilar artery, which branches into the posterior cerebral arteries.
- The anterior, middle, and posterior cerebral arteries supply blood to different regions of the brain.
- The regions and their functions are summarized in the table below.
- The anterior, middle, and posterior cerebral arteries are connected by smaller arteries called the circle of Willis. The circle of Willis provides collateral circulation in case of a blockage in one of the main arteries.
- The ABCD2 score is a tool designed to predict the risk of stroke in the 3-90 days after a TIA.
- It is based on five factors: age, blood pressure, clinical features, duration of symptoms, and diabetes.
- Each factor is assigned a score from 0 to 2. The total score ranges from 0 to 7.
- The higher the score, the higher the risk of stroke.
- The score and the corresponding risk are shown in the table below.
- The ABCD2 score can help clinicians decide whether to admit a patient with TIA to the hospital or to manage them as an outpatient.
Ischemic Stroke:
Risk Factors and Causes of Ischemic Stroke:
Pathophysiology and Clinical Manifestations of Ischemic Stroke:
Diagnostic Tests and Procedures for Ischemic Stroke:
Complications and Therapeutic Interventions for Ischemic Stroke:
Nursing Care and Education for Patients with Ischemic Stroke:
Hemorrhagic stroke
Intracerebral Hemorrhage
Subarachnoid Hemorrhage
Diagnosis of hemorrhagic stroke
Treatment of hemorrhagic stroke
Prevention of hemorrhagic stroke
Nursing Interventions of hemorrhagic stroke
Transient Ischemic Attack (TIA)
Symptoms of a Transient Ischemic Attack
Risk factors for TIA
The risk factors for TIA and ischemic stroke are similar. They include:
Diagnosis of TIA

Management of TIA
Main Arteries of the Brain
|
Artery |
Region |
Function |
|
Anterior cerebral artery |
Frontal lobe |
Personality, judgment, planning, motor control |
|
Middle cerebral artery |
Temporal lobe, parietal lobe, part of frontal lobe |
Language, speech, hearing, sensation, spatial awareness |
|
Posterior cerebral artery |
Occipital lobe, part of temporal lobe |
Vision, memory |
ABCD2 Score
|
Score |
Risk of stroke at 2 days (%) |
Risk of stroke at 90 days (%) |
|
0-3 |
1.0 |
3.1 |
|
4-5 |
4.1 |
9.8 |
|
6-7 |
8.1 |
17.8 |
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Questions on Stroke: Ischemic stroke, Hemorrhagic stroke, Transient ischemic attack (TIA)
Correct Answer is A
Explanation
Correct Answer is ["A","D","E"]
Explanation
Correct Answer is B
Explanation
Search Here
Related Topics
More on Nursing
- Pathophysiology of the Musculoskeletal System
- Pathophysiology of the Reproductive System
- Pathophysiology of the integumentary system
- Pathophysiology of the Hematologic System
- Pathophysiology of the respiratory system
- Pathophysiology of the renal system
- Pathophysiology of the Gastrointestinal System
- Basic Concepts of Pathophysiology
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
