Peripheral Nervous System Disorders: Peripheral neuropathy; Radiculopathy; Charcot-Marie-Tooth disease
- Peripheral nervous system disorders are conditions that affect the nerves outside the brain and spinal cord. They can cause sensory, motor, or autonomic dysfunction depending on the type and location of nerve damage
- Peripheral nervous system disorders can be classified as mononeuropathy or polyneuropathy based on the number of nerves involved
- Mononeuropathy is a disorder that affects a single nerve or nerve branch. It can be caused by trauma, compression, entrapment, infection, inflammation, ischemia, or toxins. Examples of mononeuropathy include carpal tunnel syndrome, radial nerve palsy, ulnar nerve palsy, peroneal nerve palsy, and Bell’s palsy
- Polyneuropathy is a disorder that affects multiple nerves in a symmetrical pattern. It can be caused by systemic diseases, metabolic disorders, immune-mediated disorders, or inherited disorders. Examples of polyneuropathy include diabetic neuropathy, alcoholic neuropathy, Guillain-Barré syndrome, and Charcot-Marie-Tooth disease
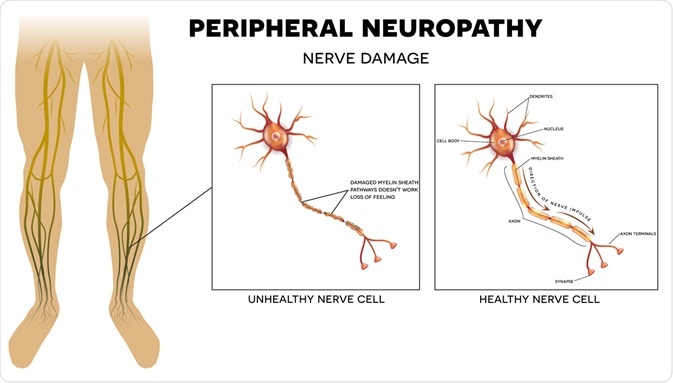
- Peripheral neuropathy is a term that encompasses any disorder that causes damage to the peripheral nerves. It can affect sensory, motor, or autonomic functions depending on the type and location of nerve damage
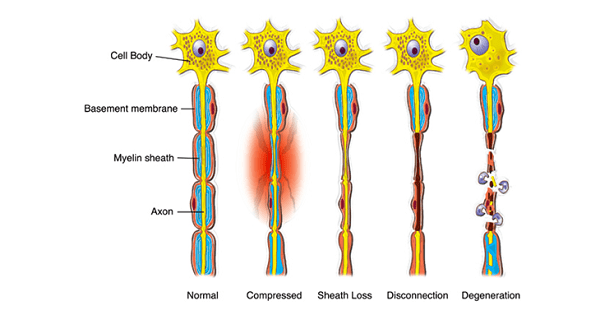
- Peripheral neuropathy can be classified as axonal or demyelinating based on the mechanism of nerve damage
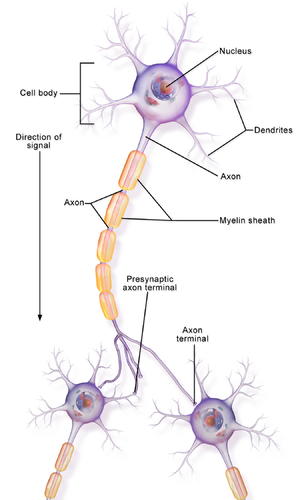
- Axonal neuropathy is caused by injury to the axon (the long projection of the neuron that carries nerve impulses). It can result from metabolic disturbances, toxic exposures, ischemia, or inflammation. Axonal neuropathy can cause symptoms such as numbness, tingling, burning, or pain in the affected nerves. It can also cause muscle weakness, atrophy, or fasciculations in the affected muscles
- Demyelinating neuropathy is caused by injury to the myelin sheath (the fatty layer that surrounds and insulates the axon). It can result from immune-mediated disorders, inherited disorders, or infections. Demyelinating neuropathy can cause symptoms such as impaired sensation, reduced reflexes, or slowed nerve conduction in the affected nerves. It can also cause muscle weakness, spasticity, or paralysis in the affected muscles
- Peripheral neuropathy can be diagnosed by a detailed history taking, physical examination, neurological assessment (including sensory testing, motor testing, reflex testing, and autonomic testing), and electrodiagnostic studies (such as nerve conduction studies [NCS] or electromyography [EMG]). Laboratory tests (such as blood glucose, electrolytes, vitamin levels, liver function tests, kidney function tests, thyroid function tests, inflammatory markers, immunological markers, and genetic tests) are also performed to identify the underlying cause of peripheral neuropathy
- Peripheral neuropathy can be treated by addressing the underlying cause (such as controlling blood glucose levels in diabetic neuropathy or avoiding alcohol intake in alcoholic neuropathy), managing the symptoms (such as using analgesics, anticonvulsants, antidepressants, or topical agents for neuropathic pain or using orthotic devices, physical therapy, or occupational therapy for muscle weakness or atrophy), and preventing complications (such as avoiding injuries, infections, or ulcers in the affected areas or maintaining good nutrition and hydration)
- Sensory neuropathy: affects the sensory nerves that carry information about sensations such as pain, temperature, touch, vibration, and position from the skin and muscles to the brain. Sensory neuropathy can cause numbness, tingling, burning, or loss of sensation in the affected areas.
- Motor neuropathy: affects the motor nerves that control the movement of muscles. Motor neuropathy can cause weakness, cramps, spasms, or paralysis of the affected muscles.
- Autonomic neuropathy: affects the autonomic nerves that regulate involuntary functions such as heart rate, blood pressure, digestion, sweating, and bladder control. Autonomic neuropathy can cause symptoms such as orthostatic hypotension, tachycardia, constipation, diarrhea, urinary retention or incontinence, erectile dysfunction, or abnormal sweating.
- Mononeuropathy: affects a single nerve or a nerve group. Mononeuropathy is usually caused by trauma, compression, or entrapment of the nerve. Examples of mononeuropathy include carpal tunnel syndrome (median nerve), ulnar nerve palsy (ulnar nerve), radial nerve palsy (radial nerve), peroneal nerve palsy (peroneal nerve), or Bell’s palsy (facial nerve).
- Multiple mononeuropathy: affects two or more nerves in different areas. Multiple mononeuropathy is usually caused by an inflammatory or ischemic process that affects several nerves. Examples of multiple mononeuropathy include vasculitis (inflammation of blood vessels), diabetic amyotrophy (diabetic nerve damage), or mononeuritis multiplex (multiple nerve inflammation).
- Polyneuropathy: affects many nerves in a symmetrical and diffuse pattern. Polyneuropathy is usually caused by a systemic or metabolic disorder that affects the entire nervous system. Examples of polyneuropathy include diabetic peripheral neuropathy (diabetic nerve damage), alcoholic neuropathy (alcohol-induced nerve damage), Guillain-Barré syndrome (acute inflammatory demyelinating polyneuropathy), or Charcot-Marie-Tooth disease (inherited demyelinating polyneuropathy).
- Acquired: develops after birth due to various factors such as diabetes, trauma, infection, autoimmune diseases, toxins, metabolic disorders, nutritional deficiencies, or cancer.
- Hereditary: inherited from one or both parents due to genetic mutations that affect the structure or function of the nerves. Examples of hereditary peripheral neuropathies include Charcot-Marie-Tooth disease (inherited demyelinating polyneuropathy), familial amyloid polyneuropathy (inherited amyloid deposition in nerves), or Fabry disease (inherited lysosomal storage disorder).
- Idiopathic: has no known cause.
- Axonal degeneration: damage to the axon (the long projection of a nerve cell that carries electrical impulses) due to ischemia (lack of blood supply), toxins (such as alcohol or chemotherapy drugs), metabolic disorders (such as diabetes or uremia), or inflammation (such as in Guillain-Barré syndrome). Axonal degeneration leads to reduced nerve conduction velocity (NCV) and reduced amplitude of action potentials.
- Demyelination: damage to the myelin sheath (the fatty layer that surrounds and insulates some axons) due to autoimmune diseases (such as Guillain-Barré syndrome or multiple sclerosis), inherited disorders (such as Charcot-Marie-Tooth disease or metachromatic leukodystrophy), or toxins (such as lead or arsenic). Demyelination leads to slowed NCV and increased latency of action potentials.
- Wallerian degeneration: damage to the distal part of the axon and the myelin sheath following a nerve injury (such as a cut or a crush). Wallerian degeneration leads to loss of nerve function and regeneration of the nerve over time.
- Sensory symptoms: numbness, tingling, burning, pain, or loss of sensation in the affected areas. Sensory symptoms usually start in the distal parts of the limbs (such as the toes or fingers) and progress proximally (towards the trunk). Sensory symptoms can affect the quality of life and increase the risk of injuries, infections, or ulcers in the affected areas.
- Motor symptoms: weakness, cramps, spasms, or paralysis of the affected muscles. Motor symptoms usually affect the proximal parts of the limbs (such as the thighs or arms) and progress distally. Motor symptoms can impair mobility and function and increase the risk of falls, fractures, or contractures in the affected areas.
- Autonomic symptoms: orthostatic hypotension (drop in blood pressure upon standing), tachycardia (fast heart rate), constipation, diarrhea, urinary retention or incontinence, erectile dysfunction, or abnormal sweating. Autonomic symptoms can affect various organ systems and cause complications such as fainting, cardiac arrhythmias, malnutrition, dehydration, or infections.
- History and physical examination: to identify the possible causes, risk factors, and characteristics of the neuropathy.
- The history should include questions about medical conditions, medications, family history, alcohol intake, nutritional status, exposure to toxins, trauma, or infections.
- The physical examination should include a neurological examination to assess the sensory, motor, and autonomic functions of the nerves.
- The physical examination should also include a skin examination to look for signs of injuries, infections, or ulcers in the affected areas.
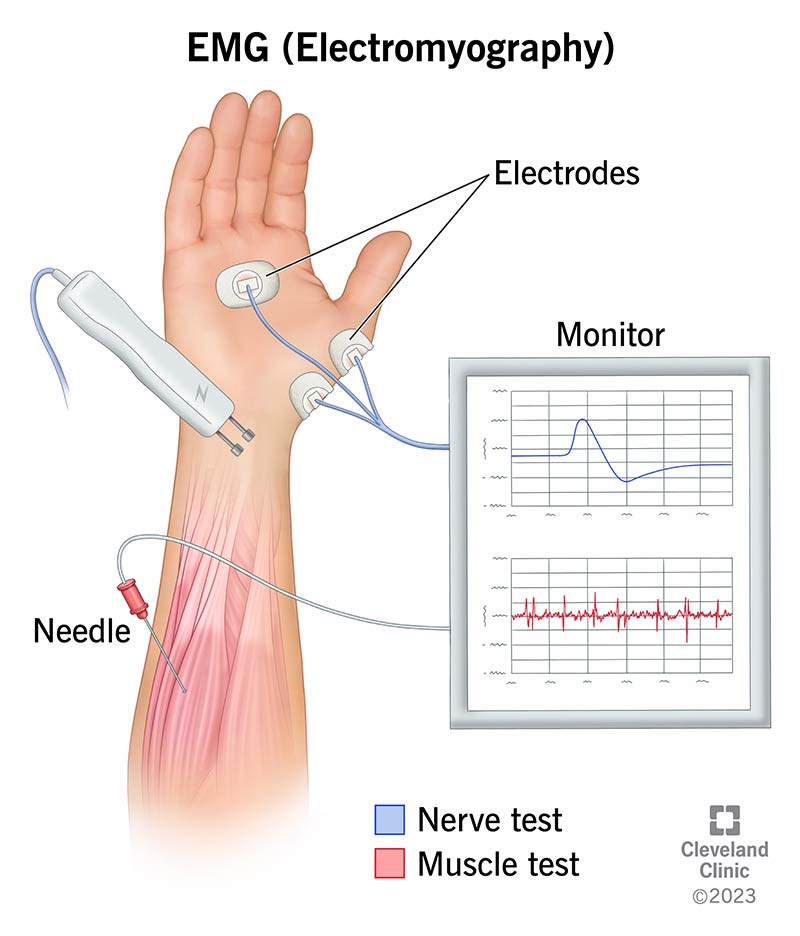
- Nerve conduction studies (NCS): to measure the NCV and amplitude of action potentials in the peripheral nerves.
- NCS can help determine the type (axonal or demyelinating), location (mononeuropathy or polyneuropathy), and severity (mild or severe) of nerve damage.
- NCS can also help differentiate between peripheral neuropathy and other neurological disorders that affect nerve function (such as myopathy or radiculopathy).
- Electromyography (EMG): to measure the electrical activity of muscles at rest and during contraction.
- EMG can help detect muscle denervation (loss of nerve supply) or reinnervation (regeneration of nerve supply) due to peripheral neuropathy.
- EMG can also help differentiate between peripheral neuropathy and other muscular disorders that affect muscle function (such as myopathy or myasthenia gravis).
- Blood tests: to identify the possible causes or complications of peripheral neuropathy.
- Blood tests may include glucose level (to diagnose diabetes), hemoglobin A1c level (to monitor diabetes control), vitamin B12 level (to diagnose vitamin B12 deficiency), thyroid function tests (to diagnose thyroid disorders), serum protein electrophoresis (to diagnose monoclonal gammopathy), erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) level (to detect inflammation), antinuclear antibody (ANA) test (to diagnose autoimmune diseases), liver function tests (to diagnose liver disorders), kidney function tests (to diagnose kidney disorders), or urine screening (to detect toxins).
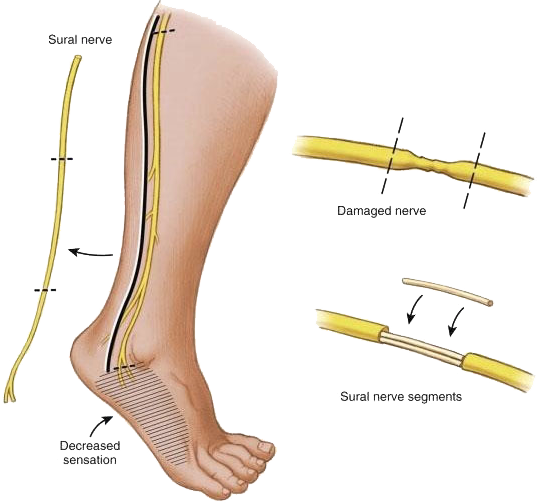
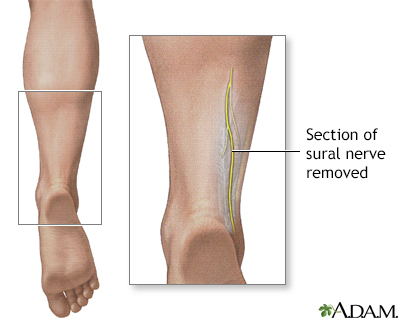
- Nerve biopsy: to obtain a sample of nerve tissue for microscopic examination.
- Nerve biopsy can help confirm the diagnosis of certain types of peripheral neuropathies that have characteristic histological features (such as vasculitis, amyloidosis, leprosy, or sarcoidosis).
- Nerve biopsy is usually reserved for cases where other diagnostic tests are inconclusive or contradictory.
- The treatment and nursing care for peripheral neuropathy depend on the cause, type, and severity of nerve damage. The general goals of treatment and nursing care are to:
- Treat the underlying cause: if possible, identify and treat the cause of peripheral neuropathy to prevent further nerve damage or complications. For example, control blood glucose level in diabetic neuropathy, avoid alcohol intake in alcoholic neuropathy, correct vitamin B12 deficiency in pernicious anemia neuropathy, use immunosuppressive drugs in autoimmune neuropathy, remove toxins in toxic neuropathy, or treat infections in infectious neuropathy.
- Manage pain: use pharmacological and non-pharmacological methods to relieve pain caused by peripheral neuropathy. Pharmacological methods
- Analgesics: drugs that reduce pain by blocking pain signals or receptors. Examples of analgesics include nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen, acetaminophen, opioids such as morphine or oxycodone, or topical agents such as lidocaine or capsaicin.
- Anticonvulsants: drugs that reduce pain by stabilizing nerve membranes and inhibiting the transmission of abnormal nerve impulses. Examples of anticonvulsants include gabapentin, pregabalin, carbamazepine, or phenytoin.
- Antidepressants: drugs that reduce pain by enhancing the activity of neurotransmitters such as serotonin and norepinephrine that modulate pain perception. Examples of antidepressants include tricyclic antidepressants such as amitriptyline or nortriptyline, selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine or paroxetine, or serotonin-norepinephrine reuptake inhibitors (SNRIs) such as duloxetine or venlafaxine.
- Physical therapy: exercises that improve muscle strength, flexibility, and coordination and prevent muscle atrophy, contractures, or deformities. Physical therapy can also include modalities such as massage, heat, cold, ultrasound, electrical stimulation, or transcutaneous electrical nerve stimulation (TENS) that improve blood circulation, reduce inflammation, or stimulate nerve regeneration.
- Occupational therapy: activities that enhance functional ability and independence in daily living tasks such as dressing, bathing, eating, or working. Occupational therapy can also include adaptive devices such as braces, splints, orthotics, or prosthetics that support or replace the function of the affected limbs.
- Cognitive-behavioral therapy (CBT): techniques that help cope with pain and improve emotional well-being by changing negative thoughts and behaviors that worsen pain. CBT can also include relaxation methods such as deep breathing, progressive muscle relaxation, guided imagery, or meditation that reduce stress and anxiety associated with pain.
- Alternative therapies: approaches that may provide relief from pain or improve quality of life by using natural or holistic methods. Examples of alternative therapies include acupuncture, acupressure, biofeedback, hypnosis, aromatherapy, herbal remedies, or dietary supplements.
- Prevent complications: monitor and manage the potential complications of peripheral neuropathy such as injuries, infections, ulcers, falls, fractures, cardiac arrhythmias, malnutrition, dehydration, or urinary tract infections. Preventive measures include:
- Educating the patient and family about the causes, symptoms, and treatment of peripheral neuropathy and the importance of regular follow-up and self-care.
- Inspecting the skin and feet daily for signs of injuries, infections, or ulcers and applying moisturizer to prevent dryness and cracking. Wearing comfortable shoes and socks and avoiding tight-fitting clothing or footwear that may cause pressure or friction. Seeking medical attention for any wounds or infections promptly.
- Using assistive devices such as a cane, walker, wheelchair, or handrails to maintain balance and prevent falls. Removing any hazards or obstacles in the home environment that may cause tripping or slipping. Wearing protective gear such as a helmet or pads when engaging in physical activities.
- Monitoring vital signs such as blood pressure, heart rate, temperature, and oxygen saturation regularly and reporting any abnormal findings to the health care provider. Taking medications as prescribed and avoiding substances that may affect the autonomic nervous system such as caffeine, alcohol, nicotine, or illicit drugs.
- Eating a balanced diet that provides adequate calories, protein, vitamins, minerals, and fluids to support nerve function and healing. Avoiding foods that may worsen neuropathy symptoms such as spicy foods, artificial sweeteners
- artificial sweeteners, or alcohol. Taking supplements that may improve nerve health such as vitamin B complex, alpha-lipoic acid, or omega-3 fatty acids as recommended by the health care provider.
- Drinking enough fluids to prevent dehydration and maintain blood volume and pressure. Avoiding sudden changes in posture that may cause orthostatic hypotension. Using compression stockings or medications that may increase blood pressure as prescribed by the health care provider.
- Emptying the bladder regularly and completely to prevent urinary retention or infection. Using catheters or medications that may improve bladder function as prescribed by the health care provider. Practicing good hygiene and avoiding irritants or allergens that may cause urinary tract infections.
- Seeking help for sexual dysfunction that may result from peripheral neuropathy. Using lubricants, devices, or medications that may enhance sexual performance or satisfaction as recommended by the health care provider. Communicating with the partner and exploring alternative ways of intimacy and pleasure.
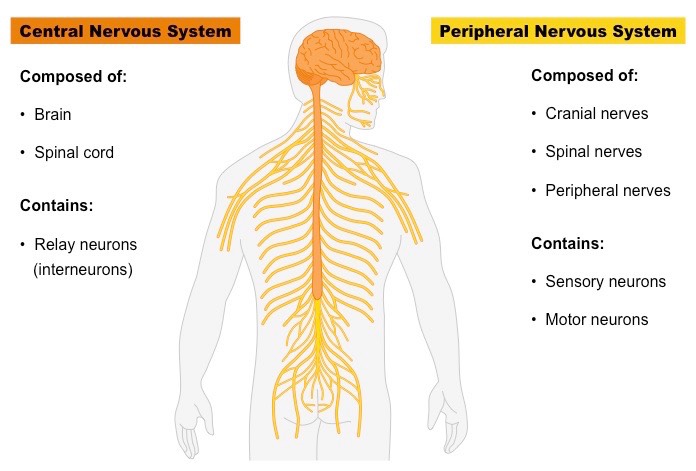
- The nervous system is a complex network of cells that communicate with each other and coordinate the functions of the body.
- It consists of two main parts: the central nervous system (CNS) and the peripheral nervous system (PNS).
- The CNS includes the brain and the spinal cord, which are protected by the skull and the vertebral column.
- The PNS includes the cranial nerves, which emerge from the brain, and the spinal nerves, which emerge from the spinal cord.
- The spinal nerves branch into smaller nerves that innervate different parts of the body.
- The nervous system can be affected by various diseases and disorders that impair its normal function and cause neurological symptoms.
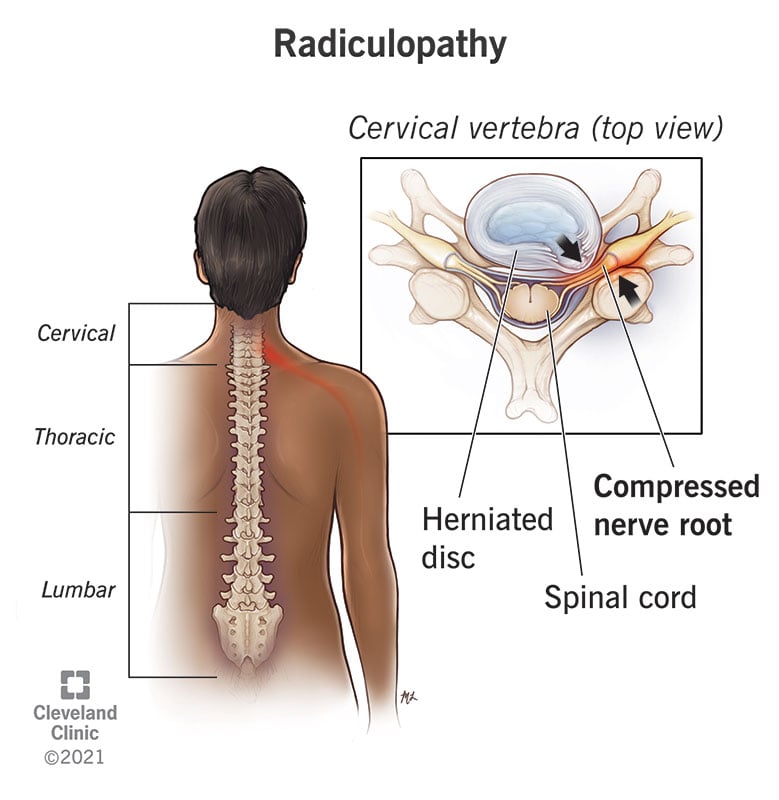
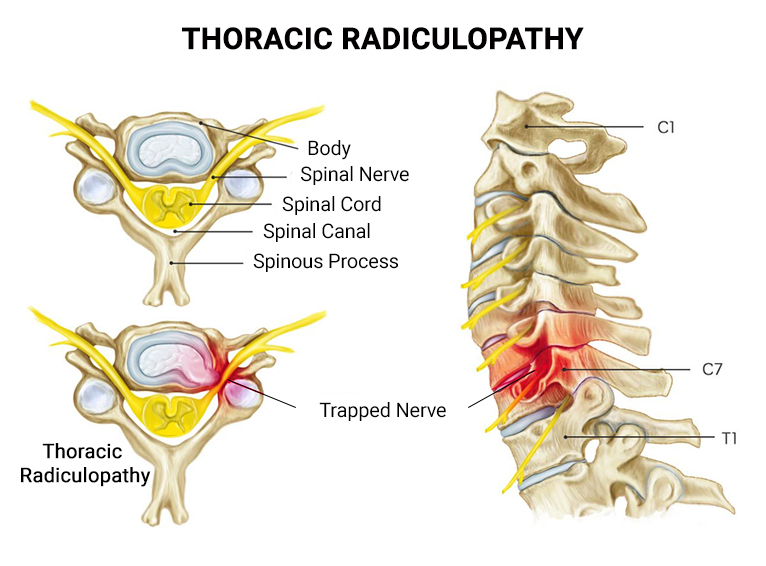
- One of these conditions is radiculopathy, which is a clinical term for a pinched or compressed nerve root in the spine.
- The nerve root is where the nerve exits the spinal cord and joins the peripheral nerve. When a nerve root is pinched, it becomes inflamed and irritated, resulting in pain, weakness, numbness, tingling, or difficulty controlling specific muscles.
- Radiculopathy can occur at any level of the spine, but it is more common in the cervical (neck) and lumbar (lower back) regions.
- Nerve injury and dysfunction can be caused by various factors, such as trauma, inflammation, infection, degeneration, compression, ischemia, toxins, or metabolic disorders.
- These factors can damage the nerve cells (neurons) or their supporting cells (glia), as well as their axons (nerve fibers) or myelin sheath (protective covering).
- Depending on the type, severity, location, and duration of the injury, nerve damage can be classified into three categories:
- Neuropraxia: This is a mild form of nerve injury that involves a temporary loss of function due to compression or ischemia of the nerve. The nerve structure remains intact, but its conduction is impaired. This type of injury usually recovers within days to weeks without permanent damage.
- Axonotmesis: This is a moderate form of nerve injury that involves a disruption of the axon and its myelin sheath due to stretching or crushing of the nerve. The nerve cell body and connective tissue remain intact, but the axon degenerates distal to the site of injury. This type of injury may recover within months to years with partial or complete regeneration of the axon.
- Neurotmesis: This is a severe form of nerve injury that involves a complete transection or rupture of the nerve due to laceration or avulsion. The nerve cell body, axon, myelin sheath, and connective tissue are all damaged beyond repair. This type of injury results in permanent loss of function and sensation.
- Radiculopathy is usually caused by compression or irritation of the nerve root due to narrowing of the space where it exits the spine.
- This can be due to various conditions that affect the spinal column, such as:
- Herniated disc: This is when a part of an intervertebral disc (a cushion between two vertebrae) protrudes out of its normal position and presses on a nearby nerve root.
- Spinal stenosis: This is when the spinal canal (the space that contains the spinal cord) or the intervertebral foramen (the opening where a nerve root exits) becomes narrowed due to bone spurs, thickened ligaments, or arthritis.
- Spondylolisthesis: This is when one vertebra slips forward over another vertebra due to a fracture or weakness in the spine.
- Spondylosis: This is a general term for degenerative changes in the spine due to aging or wear and tear.
- Spinal tumor: This is an abnormal growth of cells in or near the spine that can compress or invade a nerve root.
- Spinal infection: This is an inflammation or infection of the spine that can cause swelling or abscess formation around a nerve root.
- Spinal trauma: This is an injury to the spine due to an accident or violence that can cause fracture, dislocation, or hematoma around a nerve root.
- When a nerve root is compressed or irritated, it triggers an inflammatory response that releases chemical mediators such as prostaglandins, cytokines, histamine, bradykinin, substance P, and glutamate.
- These mediators activate nociceptors (pain receptors) on the nerve fibers and cause the transmission of pain signals to the spinal cord and the brain.
- The mediators also increase the sensitivity of the nerve fibers to mechanical, thermal, or chemical stimuli, resulting in hyperalgesia (increased pain response) and allodynia (pain response to normally non-painful stimuli).
- In addition, the compression or irritation of the nerve root can impair the conduction of motor and sensory signals along the nerve fibers, resulting in weakness, numbness, tingling, or difficulty controlling specific muscles.
- The signs and symptoms of radiculopathy depend on the level and location of the affected nerve root, as well as the type and severity of the compression or irritation.
- The most common symptom is radicular pain, which is a sharp, shooting, or burning pain that radiates along the course of the nerve from the spine to the extremity.
- The pain may be worsened by certain movements or positions of the spine, such as coughing, sneezing, bending, or twisting.
- The pain may also be accompanied by paresthesia (abnormal sensations such as tingling, pins and needles, or numbness) or dysesthesia (unpleasant sensations such as burning, itching, or electric shock).
- Other symptoms may include weakness, atrophy (wasting), or fasciculations (twitching) of the muscles innervated by the affected nerve root.
- The diagnosis of radiculopathy is based on a combination of history, physical examination, and diagnostic tests.
- The history should include information about the onset, duration, frequency, intensity, quality, location, distribution, and aggravating or relieving factors of the symptoms.
- The physical examination should include a neurological assessment that evaluates the motor function, sensory function, reflexes, and coordination of the affected area.
- The examination should also include a spinal assessment that evaluates the posture, alignment, range of motion, tenderness, deformity, and stability of the spine.
- The diagnostic tests may include:
- Imaging studies: These are used to visualize the structure and anatomy of the spine and identify any abnormalities that may cause radiculopathy. The most common imaging studies are X-rays, computed tomography (CT) scans, magnetic resonance imaging (MRI) scans, and myelography (an X-ray with contrast dye injected into the spinal canal).
- Electromyography (EMG) and nerve conduction studies (NCS): These are used to measure the electrical activity and conduction of the nerves and muscles and identify any damage or dysfunction. EMG involves inserting fine needles into the muscles and recording their electrical signals. NCS involves applying electrical stimuli to the skin over the nerves and recording their responses.
- Selective nerve root blocks (SNRB): These are used to confirm the diagnosis and provide temporary relief of radicular pain. SNRB involves injecting a local anesthetic and a steroid into a specific nerve root under fluoroscopic (X-ray) guidance. If the injection reduces or eliminates the pain, it indicates that the injected nerve root is responsible for the symptoms.
- Radiculopathy can occur at any level of the spine, but it is more common in the cervical (neck) and lumbar (lower back) regions.
- This is because these regions have more mobility and flexibility than other parts of the spine, making them more prone to injury and degeneration.
- The thoracic (upper middle back) region is less commonly affected by radiculopathy because it has less mobility and is more stabilized by the rib cage.
- The common types and locations of radiculopathy and their associated nerve roots are:
- Cervical radiculopathy: This affects the nerve roots in the cervical spine (C1-C8), which innervate the neck, shoulders, arms, hands, and fingers. The most common levels are C5-C7. The symptoms may include:
- C5 radiculopathy: Pain in the shoulder blade and outer arm; weakness in shoulder abduction (raising arm sideways) and elbow flexion (bending arm); diminished biceps reflex; numbness or tingling in thumb side of hand.
- C6 radiculopathy: Pain in the neck, shoulder blade, outer arm, thumb, index finger; weakness in elbow flexion and wrist extension (bending hand backward); diminished brachioradialis reflex; numbness or tingling in thumb index finger.
- C7 radiculopathy: Pain in the neck, shoulder blade, middle arm, middle finger; weakness in elbow extension (straightening arm) and wrist flexion (bending hand forward); diminished triceps reflex; numbness or tingling in middle finger.
- C8 radiculopathy: Pain in neck, shoulder blade, inner arm, ring and little finger; weakness in finger flexion (bending fingers) and extension (straightening fingers); diminished finger flexor reflex; numbness or tingling in ring and little finger.
- Lumbar radiculopathy: This affects the nerve roots in the lumbar spine (L1-L5), which innervate the lower back, buttocks, legs, feet, and toes. The most common levels are L4-L5 and L5-S1. The symptoms may include:
- L4 radiculopathy: Pain in the lower back, buttock, outer thigh, inner calf, and big toe; weakness in knee extension (straightening leg) and ankle dorsiflexion (lifting foot upward); diminished patellar reflex; numbness or tingling in big toe.
- L5 radiculopathy: Pain in the lower back, buttock, outer thigh, outer calf, and top of foot; weakness in hip abduction (moving leg sideways) and ankle dorsiflexion; diminished medial hamstring reflex; numbness or tingling in top of foot and toes.
- S1 radiculopathy: Pain in the lower back, buttock, back of thigh, back of calf, and outer edge of foot; weakness in hip extension (moving leg backward) and ankle plantarflexion (pushing foot downward); diminished Achilles reflex; numbness or tingling in outer edge of foot and little toe.
-
- The treatment options for radiculopathy depend on the cause, severity, duration, and location of the nerve root compression or irritation.
- The main goals of treatment are to relieve pain, reduce inflammation, restore function, and prevent complications. The treatment options may include:
- Conservative management: This involves non-surgical methods such as medication, physical therapy, exercise, massage, heat or cold therapy, acupuncture, traction, or spinal manipulation. These methods aim to reduce pain and inflammation, improve blood flow and nerve conduction, relax muscles and spasms, increase range of motion and flexibility, and strengthen muscles and posture. Conservative management is usually the first line of treatment for mild to moderate cases of radiculopathy that are not associated with severe neurological deficits or progressive symptoms.
- Interventional procedures: These involve minimally invasive methods such as injections or radiofrequency ablation. These methods aim to block or reduce pain signals from the affected nerve root by delivering a local anesthetic, a steroid, or a heat lesion. Interventional procedures are usually reserved for cases of radiculopathy that do not respond to conservative management or have severe pain that interferes with daily activities.
- Surgery: This involves invasive methods such as decompression or fusion. These methods aim to remove or stabilize the source of nerve root compression or irritation by removing a herniated disc, a bone spur, a tumor, or an infection; or by fusing two or more vertebrae together with screws, rods, plates, or cages. Surgery is usually considered as a last resort for cases of radiculopathy that have significant neurological deficits or progressive symptoms that do not improve with other treatments.
- The nursing interventions for radiculopathy are based on the assessment of the patient’s condition and the implementation of the prescribed treatment plan.
- The nursing interventions may include:
- Pain management: This involves administering analgesics (painkillers) as prescribed; monitoring pain level and response to treatment; educating the patient about pain relief options and their side effects; providing comfort measures such as positioning, massage, heat cold therapy; and encouraging relaxation techniques such as breathing exercises, meditation, or distraction.
- Neurological assessment: This involves monitoring motor function, sensory function, reflexes, and coordination of the affected area; reporting any changes or abnormalities; and documenting any neurological deficits or improvements.
- Functional assessment: This involves monitoring mobility, range of motion, strength, balance, and coordination of the affected area; assisting with activities of daily living (ADLs) such as dressing, bathing, feeding, or toileting; and providing assistive devices such as braces, splints, or crutches if needed.
- Physical therapy: This involves collaborating with the physical therapist to provide exercises, stretching, massage, traction, or spinal manipulation to the affected area; encouraging the patient to participate in the therapy sessions; and reinforcing the home exercise program.
- Patient education: This involves educating the patient about the cause, mechanism, signs symptoms of radiculopathy; the treatment options their benefits risks; the expected outcomes potential complications; the prevention strategies such as maintaining good posture, avoiding heavy lifting twisting bending of the spine; and the follow-up care such as regular check-ups imaging studies or EMG/NCS.
- Emotional support: This involves providing psychological support to the patient who may experience anxiety, depression, fear, or frustration due to radiculopathy; listening to the patient’s concerns feelings; and providing coping strategies such as counseling, support groups, or referral to a mental health professional if needed.
- Complete recovery: This is when the nerve root compression or irritation is resolved and the patient regains normal function and sensation of the affected area. This outcome is more likely for mild to moderate cases of radiculopathy that are treated early and conservatively.
- Partial recovery: This is when the nerve root compression or irritation is improved but not completely resolved and the patient has some residual symptoms or deficits of the affected area. This outcome is more common for moderate to severe cases of radiculopathy that are treated late or invasively.
- No recovery: This is when the nerve root compression or irritation is persistent or progressive and the patient has no improvement or worsening of the symptoms or deficits of the affected area. This outcome is rare but possible for severe cases of radiculopathy that are associated with irreversible nerve damage or complications.
- Complications: These are adverse events that may occur during or after the treatment of radiculopathy. They may include infection, bleeding, hematoma, nerve injury, spinal cord injury, spinal instability, failed back surgery syndrome, chronic pain, disability, or death.
- The nervous system is a complex network of cells that communicate with each other and coordinate the body’s functions1.
- The nervous system consists of two main parts: the central nervous system (CNS) and the peripheral nervous system (PNS)1.
- The CNS includes the brain and the spinal cord, which process and integrate sensory and motor information1.
- The PNS includes all the nerves that connect the CNS to the rest of the body, such as the cranial nerves, spinal nerves, and autonomic nerves1.
- The PNS can be divided into two functional categories: the somatic nervous system (SNS) and the autonomic nervous system (ANS)1.
- The SNS controls voluntary movements and sensations, such as walking, talking, seeing, hearing, etc.1
- The ANS controls involuntary functions, such as heart rate, blood pressure, digestion, etc.1
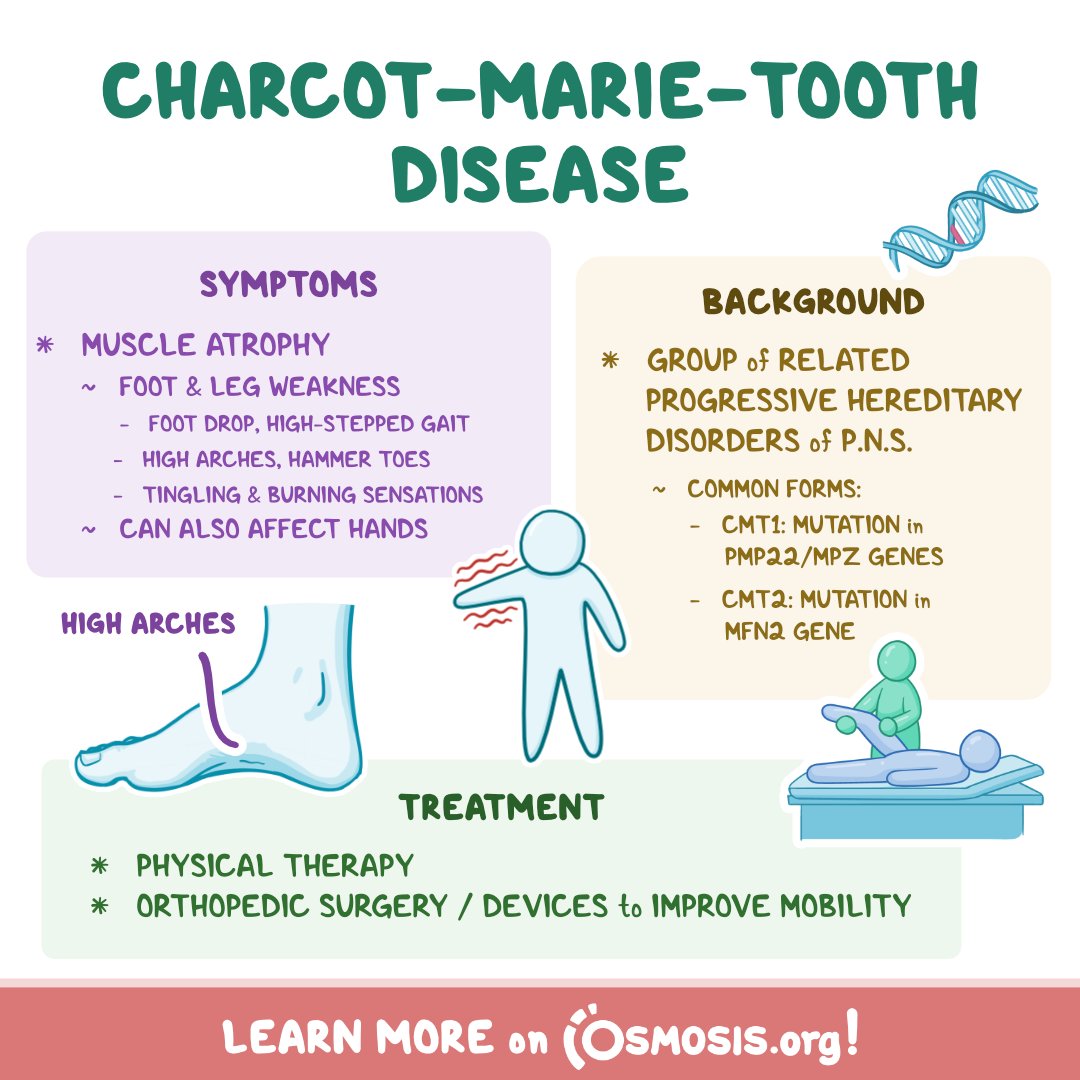
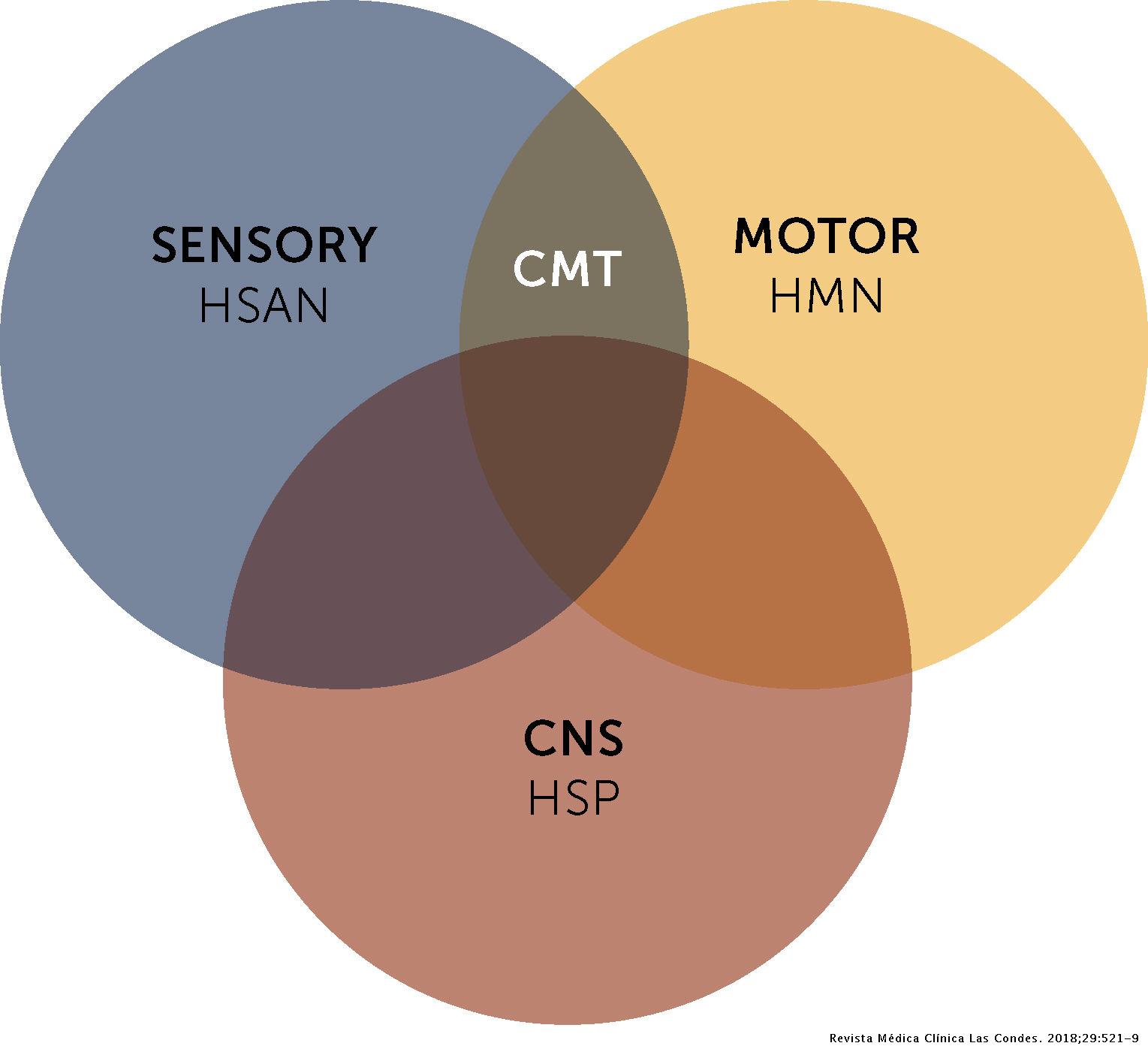
- Charcot-Marie-Tooth disease (CMT) is a group of inherited disorders that cause damage to the peripheral nerves3.
- CMT is also known as hereditary motor and sensory neuropathy (HMSN), because it affects both motor and sensory nerve fibers3.
- CMT is one of the most common inherited neurological disorders, affecting about 1 in 2500 people worldwide3.
- CMT is caused by mutations in different genes that affect either the structure or function of peripheral nerve fibers or their myelin sheath3.
- CMT can be inherited in different patterns: autosomal dominant (AD), autosomal recessive (AR), or X-linked (XL)3.
- AD means that one copy of the mutated gene from either parent is enough to cause the disease3.
- AR means that two copies of the mutated gene from both parents are needed to cause the disease3.
- XL means that the mutated gene is located on the X chromosome, which determines sex3. Males have one X chromosome and one Y chromosome, while females have two X chromosomes. Therefore, males are more likely to develop XL-CMT than females3.
- Peripheral nerves are bundles of nerve fibers that transmit signals between the CNS and the body2.
- Peripheral nerves are composed of two types of nerve fibers: motor fibers and sensory fibers2.
- Motor fibers carry impulses from the CNS to the muscles, causing them to contract2.
- Sensory fibers carry impulses from the receptors in the skin, muscles, joints, and organs to the CNS, providing information about touch, pain, temperature, position, etc.2
- Peripheral nerves are also surrounded by a protective layer called the myelin sheath2.
- Myelin is a fatty substance that insulates and speeds up the conduction of nerve impulses2.
- Myelin is produced by specialized cells called Schwann cells in the PNS and oligodendrocytes in the CNS2.
-
- CMT type 1 (CMT1) is caused by mutations in genes that affect the myelin sheath of peripheral nerves. It is usually inherited in an AD manner. It causes slow nerve conduction velocity (NCV), which measures how fast nerve impulses travel. The symptoms usually begin in childhood or adolescence. It affects both motor and sensory nerves, causing muscle weakness and atrophy, sensory loss, foot deformities, balance problems, etc.4
- CMT type 2 (CMT2) is caused by mutations in genes that affect the axons of peripheral nerves. It is usually inherited in an AD manner. It causes normal or slightly reduced NCV. The symptoms usually begin in late adolescence or adulthood. It affects mainly motor nerves, causing muscle weakness and atrophy in distal limbs. Sensory loss may be mild or absent4.
- CMT type 3 (CMT3) is also known as Dejerine-Sottas disease. It is caused by severe mutations in genes that affect the myelin sheath of peripheral nerves. It can be inherited in an AD or AR manner. It causes very slow NCV. The symptoms usually begin in infancy or early childhood. It affects both motor and sensory nerves, causing severe muscle weakness and atrophy, sensory loss, foot deformities, scoliosis, etc.4
- CMT type 4 (CMT4) is caused by mutations in genes that affect either the myelin sheath or the axons of peripheral nerves. It is inherited in an AR manner. It causes variable NCV. The symptoms usually begin in childhood or adolescence. It affects both motor and sensory nerves, causing muscle weakness and atrophy, sensory loss, foot deformities, scoliosis, etc. Some subtypes of CMT4 may also cause optic atrophy, deafness, or respiratory failure4.
- CMT type X (CMTX) is caused by mutations in genes that are located on the X chromosome. It is inherited in an XL manner. It causes variable NCV. The symptoms usually begin in childhood or adolescence. It affects both motor and sensory nerves, causing muscle weakness and atrophy, sensory loss, foot deformities, etc. Males are more severely affected than females4.
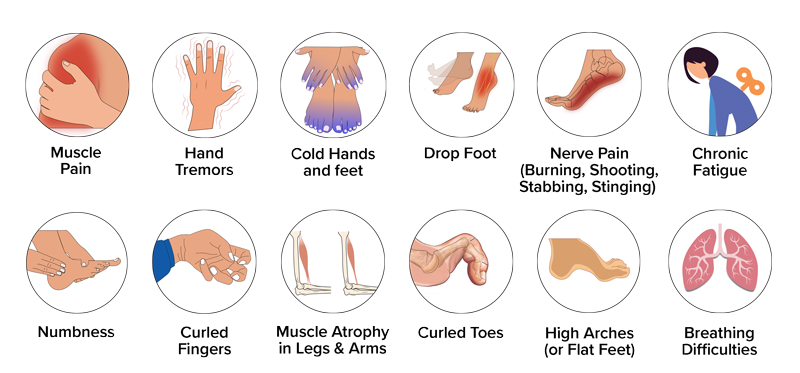
- The signs and symptoms of CMT vary depending on the type, subtype, and severity of the disease5.
- The most common signs and symptoms of CMT include5:
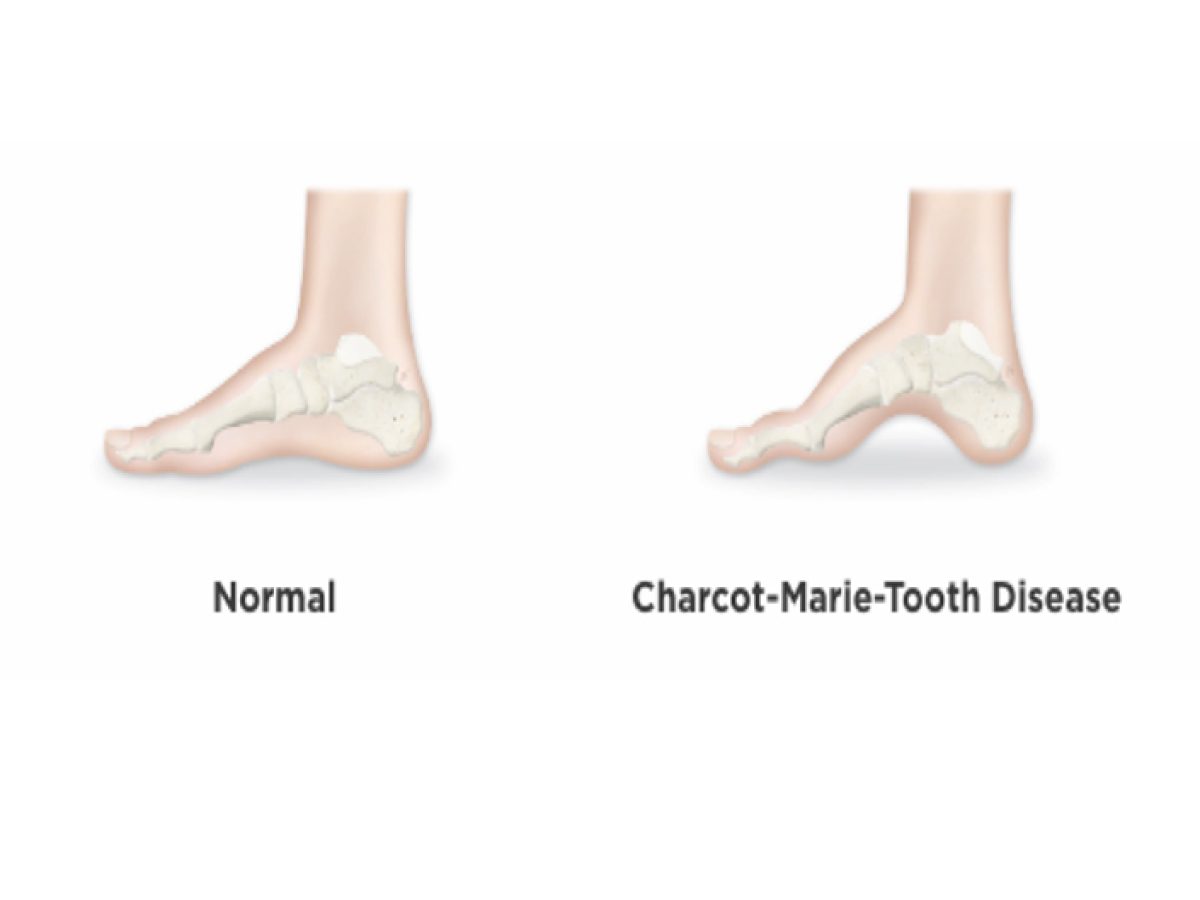
- Weakness or paralysis of the foot and lower leg muscles, which can cause difficulty lifting the foot (foot drop)
- A high-stepped gait with frequent tripping or falling
- Balance problems
- Foot deformities, such as high arches and curled toes (hammertoes)
- Lower legs may take on an "inverted champagne bottle" shape due to the loss of muscle bulk
- Reduced ability to feel heat, cold, and touch
- Weakness and atrophy may occur in the hands, causing difficulty with fine motor skills
- Decreased sense of vibration and position (proprioception)
- Curvature of the spine (scoliosis)
- Hip displacement
- Contractures (chronic shortening of muscles or tendons around joints)
- Muscle cramping
- Nerve pain
- Some individuals may need to rely on foot or leg braces or other orthopedic devices to maintain mobility5.
- Some people living with CMT experience tremor, and vision and hearing can also be affected5.
- In rare cases, breathing difficulties may occur if the nerves that control the muscles of the diaphragm are affected5.
- The severity of symptoms can vary greatly among individuals and even among family members with the disease and gene mutation5.
- The diagnosis of CMT is based on a combination of clinical examination, family history, nerve conduction studies, electromyography (EMG), nerve biopsy, and genetic testing6.
- Clinical examination involves assessing the muscle strength, reflexes, sensation, and deformities of the limbs6.
- Family history can provide clues about the inheritance pattern and type of CMT6.
- Nerve conduction studies measure the speed and amplitude of nerve impulses in different nerves6. They can help differentiate between demyelinating (CMT1) and axonal (CMT2) forms of CMT6.
- EMG measures the electrical activity of muscles at rest and during contraction6. It can help detect muscle denervation and reinnervation due to nerve damage6.
- Nerve biopsy involves taking a small sample of nerve tissue for microscopic examination6. It can show abnormalities in the myelin sheath or axons of peripheral nerves6.
- Genetic testing involves analyzing the DNA for mutations in specific genes that cause CMT6. It can confirm the diagnosis and identify the exact type and subtype of CMT6.
- There is no cure for CMT, but treatments can help manage the symptoms and improve the quality of life for patients with CMT7.
- The treatments for CMT include7:
- Physical therapy: exercises to maintain muscle strength and flexibility, prevent contractures, improve balance, etc.
- Occupational therapy: activities to improve fine motor skills, self-care abilities, etc.
- Orthotic devices: braces, splints, orthopedic shoes, etc. to support weak muscles, correct foot deformities, prevent injuries, etc.
- Surgery: procedures to correct severe foot deformities, such as high arches or hammertoes
- Medications: drugs to relieve nerve pain or muscle cramps
- Assistive devices: canes, walkers, wheelchairs, etc. to enhance mobility
- Genetic counseling: information and guidance for patients and families about the inheritance, risks, and implications of CMT
- Research: participation in clinical trials or studies to test new therapies or interventions for CMT
- The nursing care and education for patients with CMT aim to provide holistic and individualized support, promote independence and self-management, prevent complications, and enhance quality of life.
- The nursing care and education for patients with CMT include:
- Assessing the patient’s physical, psychological, social, and spiritual needs
- Monitoring the patient’s vital signs, neurological status, muscle strength, sensation, mobility, etc.
- Providing pain relief, comfort measures, wound care, infection prevention, etc.
- Assisting the patient with activities of daily living (ADLs), such as bathing, dressing, feeding, etc.
- Educating the patient and family about the nature, progression, and prognosis of CMT
- Teaching the patient and family about the available treatments and resources for CMT
- Encouraging the patient and family to adhere to the prescribed therapy regimen and follow-up appointments
- Referring the patient and family to appropriate specialists and services, such as physical therapists, occupational therapists, orthotists, surgeons, genetic counselors, social workers, etc.
- Empowering the patient and family to participate in decision-making and self-care
- Providing emotional support and counseling to the patient and family
- Advocating for the patient’s rights and preferences
- Collaborating with the interdisciplinary team to coordinate care and ensure continuity
Types and Classifications of Peripheral Neuropathy:
Peripheral neuropathy can be classified according to the type of nerve affected, the pattern of nerve involvement, or the underlying cause. According to the type of nerve affected, peripheral neuropathy can be:
According to the pattern of nerve involvement, peripheral neuropathy can be:
According to the underlying cause, peripheral neuropathy can be:
Pathophysiology of Peripheral Neuropathy:
The pathophysiology of peripheral neuropathy depends on the type and cause of nerve damage. In general, peripheral neuropathies can result from:
Clinical Manifestations and Diagnostic Tests for Peripheral Neuropathy:
The clinical manifestations of peripheral neuropathy depend on the type, location, and severity of nerve damage. The common signs and symptoms of peripheral neuropathy include:
The diagnostic tests for peripheral neuropathy include:
Treatment and Nursing Care for Peripheral Neuropathy:
Pharmacological methods include:
Non-pharmacological methods include:
Radiculopathy
Causes and Mechanisms of Nerve Injury and Dysfunction
Signs and Symptoms of Radiculopathy and How It Is Diagnosed

Common Types and Locations of Radiculopathy and Their Associated Nerve Roots
Treatment Options and Nursing Interventions for Radiculopathy
Outcomes and Potential Complications of Radiculopathy
The outcomes and potential complications of radiculopathy depend on the cause, severity, duration, and location of the nerve root compression or irritation, as well as the type and effectiveness of the treatment. The possible outcomes and complications are:
Charcot-Marie-Tooth disease
Peripheral nerves
Classification of Charcot-Marie-Tooth disease (CMT)
CMT can be classified into different types based on the genetic mutation, inheritance pattern, clinical features, and nerve conduction studies4.
Signs and symptoms of CMT
Diagnosis of CMT
Treatment of CMT
Nursing care and education for patients with CMT
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Questions on Peripheral Nervous System Disorders: Peripheral neuropathy; Radiculopathy; Charcot-Marie-Tooth disease
Correct Answer is A
Explanation
Correct Answer is ["A","B","C","D"]
Explanation
Correct Answer is C
Explanation
Search Here
Related Topics
More on Nursing
- Pathophysiology of the Musculoskeletal System
- Pathophysiology of the Reproductive System
- Pathophysiology of the integumentary system
- Pathophysiology of the Hematologic System
- Pathophysiology of the respiratory system
- Pathophysiology of the renal system
- Pathophysiology of the Gastrointestinal System
- Basic Concepts of Pathophysiology
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
