Neuroinflammation: Multiple sclerosis; Meningitis; Guillain-Barré syndrome
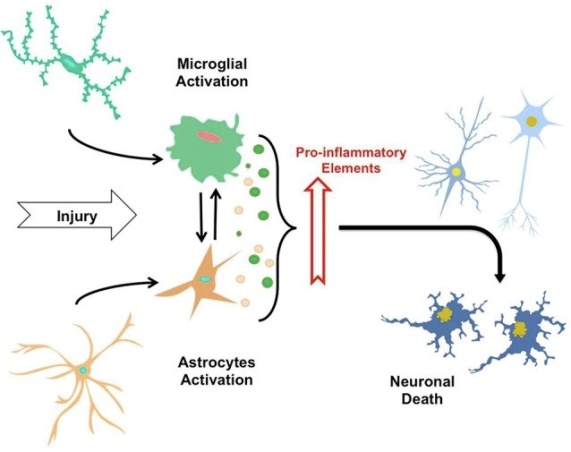
- Neuroinflammation is a pathological process that involves the activation of the immune system in response to injury or infection in the nervous system
- Neuroinflammation can be beneficial or harmful depending on the type, duration, and intensity of the immune response
- Beneficial neuroinflammation can promote tissue repair and regeneration by removing debris, releasing growth factors, and stimulating neurogenesis (the formation of new neurons)
- Harmful neuroinflammation can cause tissue damage and dysfunction by releasing pro-inflammatory cytokines (chemical messengers), reactive oxygen species (free radicals), and excitatory neurotransmitters (e.g., glutamate) that can induce neuronal death, demyelination (the loss of the myelin sheath that insulates axons), and synaptic dysfunction (the impairment of communication between neurons)
- Neuroinflammation can be triggered by various factors such as trauma, stroke, tumors, infections, autoimmune diseases, etc.
- Neuroinflammation can result in various neurological disorders such as:
- multiple sclerosis (MS),
- meningitis,
- Guillain-Barré syndrome (GBS)
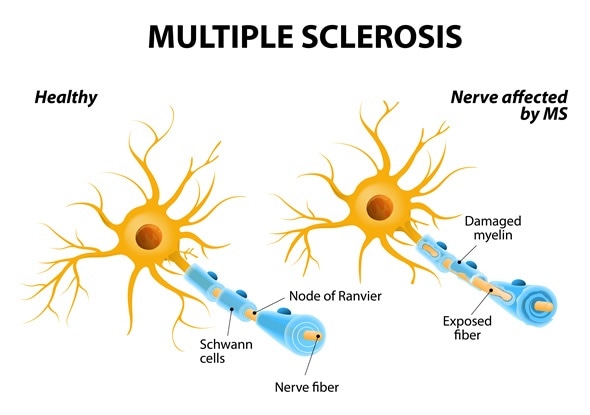
- MS is a chronic autoimmune disease that affects the CNS. It is characterized by the formation of inflammatory lesions or plaques in the white matter of the brain and spinal cord, leading to demyelination and axonal damage
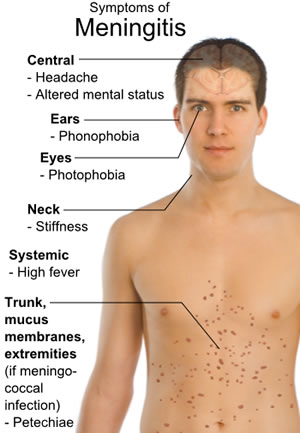
- Meningitis is an acute infection that affects the meninges (the membranes that cover the brain and spinal cord). It is caused by various microorganisms such as bacteria, viruses, fungi, parasites, etc. that enter the CNS through the bloodstream or direct contact. It is characterized by inflammation of the meninges, leading to headache, fever, neck stiffness, photophobia (sensitivity to light), altered mental status, etc.
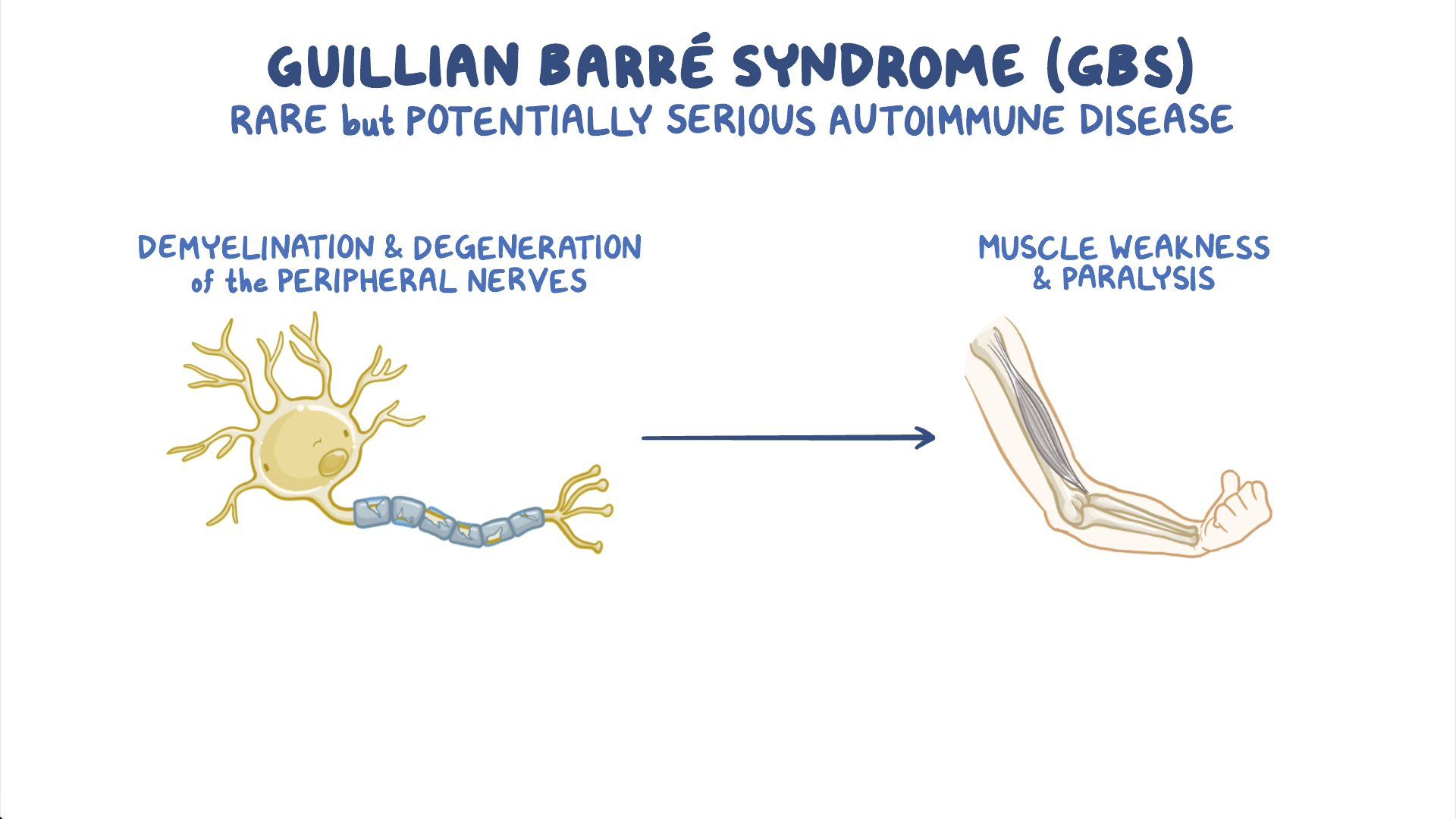
- GBS is an acute inflammatory polyneuropathy (a disorder that affects multiple peripheral nerves). It is caused by an abnormal immune response to a preceding infection or vaccination that targets the myelin or axons of the peripheral nerves. It is characterized by ascending weakness or paralysis of the limbs, face, and respiratory muscles, leading to difficulty in walking, speaking, swallowing, breathing, etc.
- MS is a chronic and unpredictable disease of the central nervous system (CNS), which consists of the brain, spinal cord, and optic nerves 12
- In MS, the immune system mistakenly attacks the protective covering (myelin) of nerve fibers, causing inflammation, damage, and scar tissue (sclerosis or lesions) 123
- The damage to the nerve fibers disrupts the communication between the brain and the rest of the body, resulting in various symptoms that depend on the location and extent of the lesions 123
- The cause of MS is unknown, but it is likely influenced by a combination of genetic and environmental factors, such as infections, vitamin D deficiency, smoking, or exposure to toxins 123
- MS affects people differently and can have a wide range of symptoms, such as numbness, tingling, weakness, fatigue, vision problems, balance problems, coordination problems, bladder problems, bowel problems, cognitive problems, mood problems, pain, and spasticity 123
- MS is diagnosed based on the signs and symptoms, medical history, physical examination, blood tests, and imaging tests such as magnetic resonance imaging (MRI) or optical coherence tomography (OCT) 123
- There are four main types of MS based on the pattern of symptoms over time: relapsing-remitting MS (RRMS), secondary-progressive MS (SPMS), primary-progressive MS (PPMS), and progressive-relapsing MS (PRMS) 123
- There is no cure for MS, but there are treatments that can help reduce the frequency and severity of relapses, slow down the progression of the disease, manage the symptoms, and improve the quality of life. These treatments include disease-modifying therapies (DMTs), corticosteroids, symptom management medications, rehabilitation therapies, complementary and alternative therapies, and lifestyle modifications 123
- MS is more common in women than in men and usually affects people between the ages of 20 and 50. It is estimated that about 2.8 million people worldwide have MS. The prevalence of MS varies by geographic region, with higher rates in temperate zones than in tropical zones 12
- Causes: The exact cause of multiple sclerosis (MS) is unknown. However, some possible factors that may trigger or contribute to the development of MS include
- genetic susceptibility,
- environmental exposure (e.g., vitamin D deficiency, smoking, infection),
- immune dysregulation (e.g., molecular mimicry, epitope spreading, bystander activation) that lead to the activation of autoreactive T cells and B cells that cross the blood-brain barrier (BBB) and attack the myelin and axons of the CNS
- Risk factors:
- age (20-50 years),
- sex (female),
- race (white),
- family history,
- geography (higher prevalence in temperate regions),
- certain infections (e.g., Epstein-Barr virus, human herpesvirus 6, etc.)
- Signs and symptoms: The signs and symptoms of MS vary depending on the location and extent of the lesions or plaques in the CNS.
- Some common manifestations include:
- sensory disturbances (e.g., numbness, tingling, pain)
- motor weakness or spasticity
- visual impairment or optic neuritis (inflammation of the optic nerve)
- fatigue
- cognitive impairment or dementia
- emotional changes or depression
- bladder or bowel dysfunction
- sexual dysfunction
- Diagnosis: The diagnosis of MS is based on clinical criteria that include evidence of dissemination in space (DIS) and dissemination in time (DIT) of CNS lesions that are consistent with MS and not better explained by other conditions. Some diagnostic tests that may be used to support the diagnosis or rule out other causes include:
- Neuroimaging: To visualize the structure and function of the brain and spinal cord using techniques such as MRI, PET, SPECT, etc. that may show multiple lesions or plaques in different regions and stages of MS
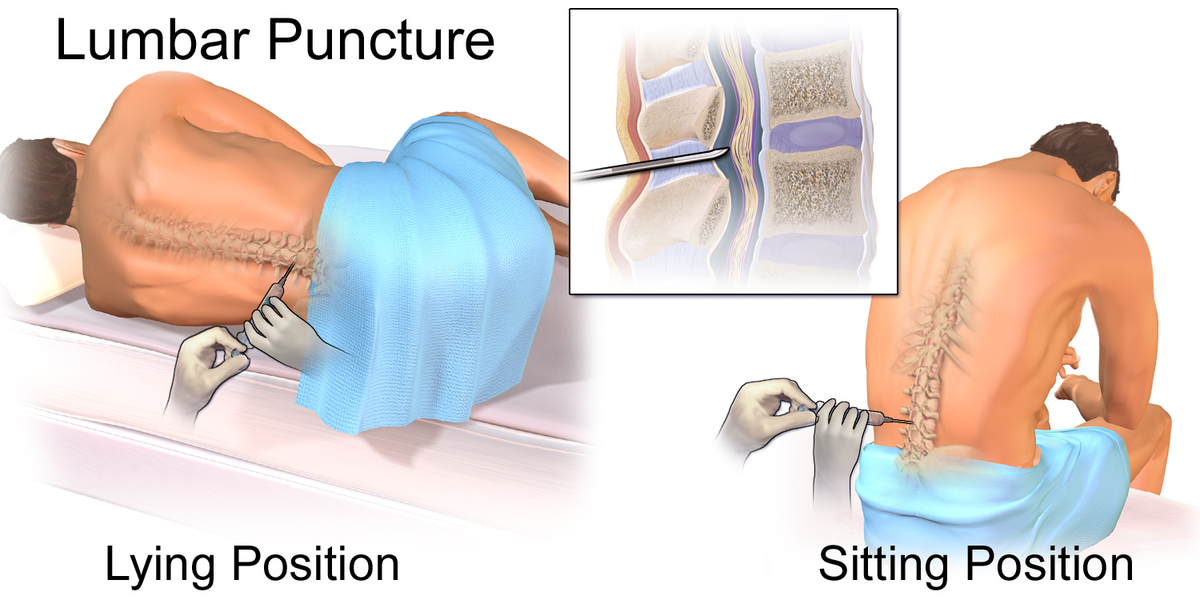
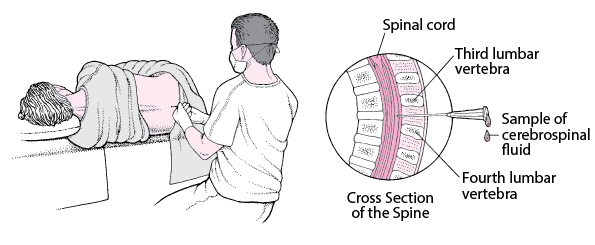
- Lumbar puncture: To measure the levels of immunoglobulin G (IgG) and oligoclonal bands (OCBs) in the CSF that may indicate an immune response in the CNS
- Evoked potentials: To measure the electrical activity of the brain in response to sensory stimuli such as visual, auditory, or somatosensory stimuli that may show delayed or reduced responses due to demyelination
- Blood tests: To check for infection, inflammation, autoantibodies, etc. that may cause or mimic MS
- Treatment: The treatment of MS is aimed at modifying the course of the disease, managing the symptoms, preventing relapses, and improving the quality of life. Some treatment options include:
- Disease-modifying therapies (DMTs): To reduce the frequency and severity of relapses and delay the progression of disability using drugs such as interferons (e.g., interferon beta-1a, interferon beta-1b), glatiramer acetate, natalizumab, fingolimod, alemtuzumab, ocrelizumab, etc. that modulate the immune system by inhibiting T cell activation, migration, or proliferation; reducing inflammation; or depleting B cells. These drugs may have side effects such as injection site reactions, flu-like symptoms, liver toxicity, infection risk, etc.
- Symptomatic therapies: To manage or reduce specific symptoms such as spasticity, pain, fatigue, depression, bladder dysfunction, etc. using drugs such as baclofen, tizanidine, gabapentin, amitriptyline, modafinil, fluoxetine, oxybutynin, etc. that act on various neurotransmitter systems or receptors to relax muscles, relieve pain, enhance energy, improve mood, control urination, etc.
- Rehabilitation therapies: To improve or maintain physical function and mobility using interventions such as exercise, stretching, balance training, gait training, etc. that involve performing physical activities that are appropriate for the patient’s condition and preferences. These interventions may prevent or delay complications such as falls, fractures, pressure ulcers, contractures, etc. and improve cardiovascular health, muscle strength, flexibility, and endurance in MS patients
- Occupational therapy: To improve or maintain daily living skills and independence using interventions such as task analysis, task simplification, assistive devices, environmental adaptation, etc. that involve breaking down complex tasks into simpler steps, reducing the cognitive demands of tasks, providing aids or tools to facilitate tasks, modifying the environment to suit the patient’s needs and abilities, etc. These interventions may enhance self-care,productivity,leisure,and safety in MS patients - Speech therapy: To improve or maintain communication and swallowing skills using interventions such as language stimulation,cueing,prompting,AAC devices,swallowing exercises,diet modification,etc. that involve providing verbal or non-verbal cues to elicit responses,repeating or rephrasing words or sentences,using pictures or symbols to convey messages,performing oral motor exercises to strengthen the muscles involved in swallowing,changing the texture or consistency of food or liquids to facilitate swallowing,etc. These interventions may prevent or reduce communication difficulties,social isolation,aspiration pneumonia,malnutrition,dehydration,etc. in MS patients
- Cognitive therapy: To improve or maintain cognitive abilities and function using interventions such as cognitive stimulation therapy (CST), cognitive rehabilitation, cognitive behavioral therapy (CBT), etc. that involve engaging in meaningful activities, training specific cognitive domains, addressing psychological issues, etc. These interventions may enhance memory, attention, language, executive functions, etc. and improve mood, self-esteem, coping skills, etc. in MS patients - Prevention: The prevention of MS is not fully established. However, some possible preventive measures include avoiding smoking, maintaining adequate vitamin D levels, avoiding infections, and following a healthy lifestyle
- Meningitis is an inflammation of the meninges, which are the protective layers surrounding the brain and spinal cord 12
- Meningitis can be life-threatening and requires immediate medical attention, especially if it is caused by bacteria, which can lead to serious complications, such as brain damage, hearing loss, or death 124
- The symptoms of meningitis may vary depending on the cause and age of the person, but they often include fever, headache, stiff neck, nausea, vomiting, confusion, sensitivity to light, and skin rash 124
- Meningitis can be caused by various types of infections, such as bacteria, viruses, fungi, and parasites, as well as non-infectious conditions, such as cancer, drugs, or autoimmune disorders 123
- Causes: The causes of meningitis vary depending on the type of microorganism that infects the meninges. Some common causes include:
- Bacterial meningitis: Caused by bacteria such as Streptococcus pneumoniae (pneumococcus), Neisseria meningitidis (meningococcus), Haemophilus influenzae type b (Hib), Listeria monocytogenes, etc. that enter the CNS through the bloodstream or direct contact (e.g., respiratory droplets, contaminated food, etc.)
- Viral meningitis: Caused by viruses such as enteroviruses (e.g., coxsackievirus, echovirus), herpes simplex virus (HSV), varicella-zoster virus (VZV), mumps virus, etc. that enter the CNS through the bloodstream or direct contact (e.g., saliva, blisters, etc.)
- Fungal meningitis: Caused by fungi such as Cryptococcus neoformans, Candida albicans, Histoplasma capsulatum, etc. that enter the CNS through the bloodstream or direct contact (e.g., inhalation of spores, skin contact with infected animals, etc.)
- Parasitic meningitis: Caused by parasites such as Naegleria fowleri, Acanthamoeba spp., Angiostrongylus cantonensis, etc. that enter the CNS through the bloodstream or direct contact (e.g., nasal irrigation with contaminated water, ingestion of raw or undercooked snails or slugs, etc.)
- Risk factors: Some factors that may increase the risk of developing meningitis include age (infants and young children), immunocompromised status (e.g., HIV/AIDS, cancer, transplantation, etc.), close contact with infected individuals or animals, travel to endemic areas, lack of vaccination, etc.
- Signs and symptoms: The signs and symptoms of meningitis vary depending on the type and severity of the infection.
- headache
- fever
- neck stiffness
- photophobia
- altered mental status
- nausea
- vomiting
- rash
- seizures
- Diagnosis: The diagnosis of meningitis is based on clinical criteria that include medical history, physical examination, neurological examination, and exclusion of other possible causes. Some diagnostic tests that may be used to confirm the diagnosis or identify the causative agent include:
- Lumbar puncture: To obtain a sample of CSF for analysis and culture that may show increased pressure, increased white blood cell count (WBC), decreased glucose level, increased protein level, and presence of bacteria, viruses, fungi, or parasites
- Blood tests: To check for infection, inflammation, blood culture, etc. that may show increased WBC, increased erythrocyte sedimentation rate (ESR), increased C-reactive protein (CRP), and presence of bacteria, viruses, fungi, or parasites
- Urine tests: To check for infection and culture that may show presence of bacteria, viruses, fungi, or parasites
- Neuroimaging: To visualize the structure and function of the brain and spinal cord using techniques such as CT, MRI, PET, SPECT, etc. that may show inflammation of the meninges or other complications such as abscesses, hydrocephalus (excess fluid in the brain), cerebral edema (swelling of the brain), etc.
- Treatment: The treatment of meningitis is aimed at eradicating the infection, reducing the inflammation, managing the symptoms, preventing complications, and improving the outcome. Some treatment options include:
- Antibiotics: To treat bacterial meningitis using drugs such as penicillin, ceftriaxone, vancomycin, etc. that target the specific type of bacteria causing the infection. These drugs may have side effects such as allergic reactions, diarrhea, kidney toxicity, etc.
- Antivirals: To treat viral meningitis using drugs such as acyclovir, ganciclovir, etc. that inhibit the replication of the virus causing the infection. These drugs may have side effects such as nausea, vomiting, headache, etc.
- Antifungals: To treat fungal meningitis using drugs such as amphotericin B, fluconazole, etc. that interfere with the cell membrane or synthesis of the fungus causing the infection. These drugs may have side effects such as fever, chills, kidney toxicity, liver toxicity, etc.
- Antiparasitics: To treat parasitic meningitis using drugs such as albendazole, ivermectin, etc. that kill or paralyze the parasite causing the infection. These drugs may have side effects such as abdominal pain, dizziness, rash, etc.
- Corticosteroids: To reduce the inflammation and swelling of the meninges and brain using drugs such as dexamethasone, prednisone, etc. that suppress the immune system and inhibit the production of pro-inflammatory cytokines. These drugs may have side effects such as increased blood pressure, increased blood sugar, increased risk of infection, etc.
- Analgesics: To relieve pain and fever using drugs such as acetaminophen, ibuprofen, etc. that block the production of prostaglandins (chemical messengers) that mediate pain and inflammation. These drugs may have side effects such as stomach irritation, bleeding, liver toxicity, kidney toxicity, etc.
- Anticonvulsants: To prevent or control seizures using drugs such as phenytoin, carbamazepine, valproic acid, etc. that stabilize the electrical activity of the brain by modulating sodium, calcium, or potassium channels or enhancing gamma-aminobutyric acid (GABA) activity. These drugs may have side effects such as drowsiness, dizziness, rash, liver toxicity, etc.
- Fluids and electrolytes: To maintain hydration and electrolyte balance using intravenous fluids that contain water, sodium, potassium, chloride, bicarbonate, etc. that regulate the osmolarity, pH, and volume of body fluids
- Oxygen therapy: To provide adequate oxygenation and ventilation using devices such as nasal cannula, face mask, ventilator, etc. that deliver oxygen to the lungs and remove carbon dioxide from the body
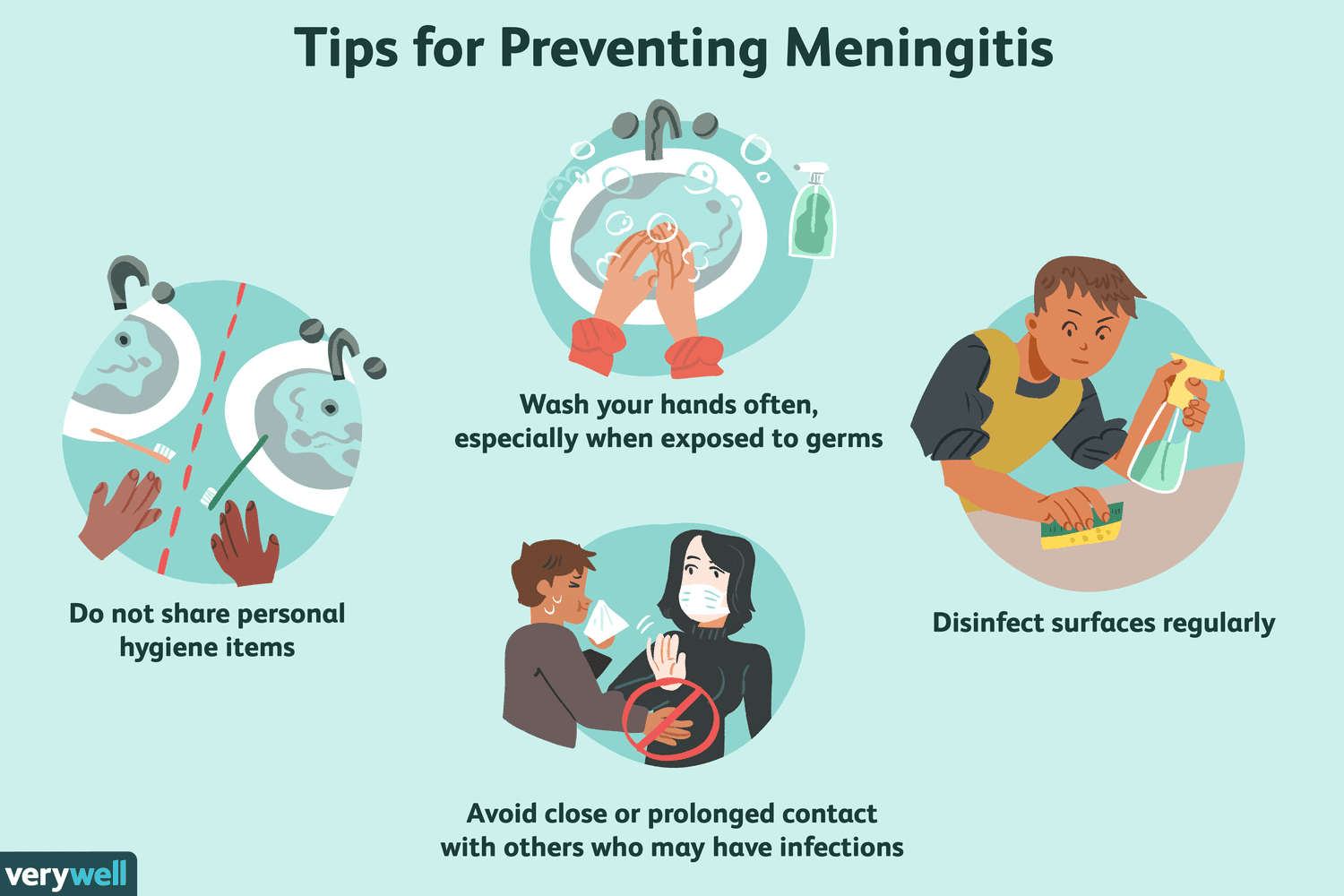
- Prevention: The prevention of meningitis depends on the type and source of infection.
- Some preventive measures include
- vaccination against common causes of bacterial or viral meningitis (e.g., pneumococcal vaccine, meningococcal vaccine, Hib vaccine, MMR vaccine, etc.),
- avoiding close contact with infected individuals or animals,
- practicing good hygiene (e.g., washing hands, covering mouth and nose when coughing or sneezing, etc.),
- avoiding contaminated food or water (e.g., cooking food thoroughly, boiling or filtering water, etc.)
- seeking medical attention if experiencing any signs or symptoms of meningitis
- GBS is a rare but serious autoimmune disorder in which the immune system mistakenly attacks healthy nerve cells in the peripheral nervous system (PNS) 12
- The PNS is the network of nerves located outside of the brain and spinal cord that control sensory, motor, and autonomic functions 13
- The immune attack causes inflammation and damage to the myelin sheaths that protect and insulate the nerve fibers, resulting in impaired transmission of nerve impulses 24
- The exact cause of GBS is unknown, but it is often triggered by an infection, such as COVID-19, respiratory or gastrointestinal infection, or Zika virus, or less commonly by surgery or vaccination 24
- GBS can be life-threatening if it affects the breathing muscles or the autonomic nervous system, which can cause dangerous abnormalities in heart rate and blood pressure 12
- The diagnosis of GBS is based on the signs and symptoms, nerve conduction studies that measure the speed and strength of nerve signals, and lumbar puncture that examines the cerebrospinal fluid for elevated protein levels 24
- There are several subtypes of GBS based on the areas of weakness, results of nerve conduction studies, and the presence of certain antibodies. The most common subtype in North America and Europe is acute inflammatory demyelinating polyradiculoneuropathy (AIDP), while other subtypes include Miller Fisher syndrome (MFS), acute motor axonal neuropathy (AMAN), and acute motor-sensory axonal neuropathy (AMSAN) 25
- There is no cure for GBS, but treatments can ease symptoms and reduce the duration of the illness. The main treatments are intravenous immunoglobulins (IVIG) or plasmapheresis (plasma exchange), which both aim to remove harmful antibodies from the blood. Supportive care may include mechanical ventilation, pain management, physical therapy, and psychological support 24
- Most people with GBS recover completely or have only mild residual weakness. Recovery may take weeks to years, with about a third having some permanent weakness. About 15% of people have a relapse of muscle weakness or sensory symptoms. The mortality rate of GBS is about 7.5%, mainly due to complications such as infections, blood clots, or cardiac arrest 124
- GBS is rare, affecting about 1 or 2 people per 100,000 every year. It can affect anyone at any age and any gender. It was first described by French neurologists Georges Guillain and Jean Alexandre Barré in 1916 2
- Causes: The exact cause of GBS is unknown.
- However, some possible factors that may trigger or contribute to the development of GBS include
- preceding infection (e.g., Campylobacter jejuni, cytomegalovirus (CMV), Epstein-Barr virus (EBV), Zika virus, etc.), vaccination (e.g., influenza vaccine), surgery, trauma, etc. that induce an abnormal immune response that cross-reacts with the myelin or axons of the peripheral nerves
- Risk factors: Some factors that may increase the risk of developing GBS include age (older adults), sex (male), genetics (e.g., HLA alleles), immunocompromised status (e.g., HIV/AIDS), etc.
- Signs and symptoms: The signs and symptoms of GBS vary depending on the type and severity of the nerve damage.
- Some common manifestations include ascending weakness or paralysis of the limbs, face, and respiratory muscles; sensory disturbances (e.g., numbness, tingling, pain);
- autonomic dysfunction (e.g., blood pressure fluctuations, heart rate abnormalities, sweating abnormalities);
- cranial nerve involvement (e.g., facial palsy, ophthalmoplegia (eye movement paralysis), dysphagia (difficulty swallowing), dysarthria (difficulty speaking)); etc.
- Diagnosis: The diagnosis of GBS is based on clinical criteria that include medical history, physical examination, neurological examination, and exclusion of other possible causes. Some diagnostic tests that may be used to support the diagnosis or rule out other conditions include:
- Lumbar puncture: To obtain a sample of CSF for analysis that may show increased protein level and normal WBC count (albuminocytologic dissociation) that indicate nerve damage
- Nerve conduction studies (NCS) and electromyography (EMG): To measure the electrical activity and function of the peripheral nerves and muscles that may show reduced nerve conduction velocity, prolonged distal latency, reduced amplitude, and abnormal spontaneous activity that indicate demyelination or axonal degeneration
- Blood tests: To check for infection, inflammation, autoantibodies, etc. that may cause or mimic GBS
- Treatment: The treatment of GBS is aimed at stopping the immune attack, supporting the vital functions, managing the symptoms, preventing complications, and promoting recovery. Some treatment options include:
- Immunotherapy: To reduce the immune response and remove the harmful antibodies using methods such as plasma exchange (PE) or intravenous immunoglobulin (IVIG) that involve removing or diluting the patient’s plasma (the liquid part of blood that contains antibodies) and replacing it with fresh plasma or immunoglobulin (a solution of antibodies) that can neutralize or block the harmful antibodies. These methods may have side effects such as allergic reactions, infection risk, fluid overload, etc.
- Supportive therapy: To provide adequate oxygenation and ventilation using devices such as nasal cannula, face mask, ventilator, etc. that deliver oxygen to the lungs and remove carbon dioxide from the body; to maintain hydration and electrolyte balance using intravenous fluids that contain water, sodium, potassium, chloride, bicarbonate, etc. that regulate the osmolarity, pH, and volume of body fluids; to prevent or treat infections using antibiotics or antivirals that target the specific type of microorganism causing the infection; to prevent or treat thromboembolism (blood clot formation) using anticoagulants (e.g., heparin, warfarin, etc.) that inhibit the coagulation cascade or thrombolytics (e.g., streptokinase, tissue plasminogen activator (tPA), etc.) that dissolve existing clots
- Symptomatic therapy: To manage or reduce specific symptoms such as pain, spasticity, autonomic dysfunction, etc. using drugs such as gabapentin, baclofen, midodrine, etc. that act on various neurotransmitter systems or receptors to relieve pain, relax muscles, increase blood pressure, etc.
- Rehabilitation therapy: To improve or maintain physical function and mobility using interventions such as exercise, stretching, balance training, gait training, etc. that involve performing physical activities that are appropriate for the patient’s condition and preferences. These interventions may prevent or delay complications such as contractures, muscle atrophy, pressure ulcers, etc. and improve muscle strength, flexibility, and endurance in GBS patients
- Occupational therapy: To improve or maintain daily living skills and independence using interventions such as task analysis, task simplification, assistive devices, environmental adaptation, etc. that involve breaking down complex tasks into simpler steps, reducing the cognitive demands of tasks, providing aids or tools to facilitate tasks, modifying the environment to suit the patient’s needs and abilities, etc. These interventions may enhance self-care, productivity, leisure, and safety in GBS patients
- Speech therapy: To improve or maintain communication and swallowing skills using interventions such as language stimulation, cueing, prompting, AAC devices, swallowing exercises, diet modification, etc. that involve providing verbal or noverbal cues to elicit responses, repeating or rephrasing words or sentences, using pictures or symbols to convey messages, performing oral motor exercises to strengthen the muscles involved in swallowing, changing the texture or consistency of food or liquids to facilitate swallowing, etc. These interventions may prevent or reduce communication difficulties, social isolation, aspiration pneumonia, malnutrition, dehydration, etc. in GBS patients
- Prevention: The prevention of GBS is not fully established. However, some possible preventive measures include avoiding infections or vaccinations that may trigger GBS, practicing good hygiene (e.g., washing hands), and seeking medical attention if experiencing any signs or symptoms of GBS
multiple sclerosis (MS)
Causes and Risk factors of multiple sclerosis (MS)
Risk factors of multiple sclerosis (MS)
Signs and symptoms of multiple sclerosis (MS)
Diagnosis of multiple sclerosis (MS)
Treatment of multiple sclerosis (MS)
Meningitis
Causes and Risk factors of Menengitis
Signs and symptoms of Meningitis
Diagnosis of Meningitis
Treatment of Meningitis
Prevention of Meningitis
Guillain-Barré syndrome (GBS)
Causes and risk factors of GBS
Signs and symptoms of GBS
Diagnosis and symptoms of GBS
Treatment and prevention of GBS
Nursing Test Bank
Quiz #1: RN Exams Pharmacology Exams
Quiz #2: RN Exams Medical-Surgical Exams
Quiz #3: RN Exams Fundamentals Exams
Quiz #4: RN Exams Maternal-Newborn Exams
Quiz #5: RN Exams Anatomy and Physiology Exams
Quiz #6: RN Exams Obstetrics and Pediatrics Exams
Quiz #7: RN Exams Fluid and Electrolytes Exams
Quiz #8: RN Exams Community Health Exams
Quiz #9: RN Exams Promoting Health across the lifespan Exams
Quiz #10: RN Exams Multidimensional care Exams
Naxlex Comprehensive Predictor Exams
Quiz #1: Naxlex RN Comprehensive online practice 2019 B with NGN
Quiz #2: Naxlex RN Comprehensive Predictor 2023
Quiz #3: Naxlex RN Comprehensive Predictor 2023 Exit Exam A
Quiz #4: Naxlex HESI Exit LPN Exam
Quiz #5: Naxlex PN Comprehensive Predictor PN 2020
Quiz #6: Naxlex VATI PN Comprehensive Predictor 2020
Quiz #8: Naxlex PN Comprehensive Predictor 2023 - Exam 1
Quiz #10: Naxlex HESI PN Exit exam
Quiz #11: Naxlex HESI PN EXIT Exam 2
Questions on Neuroinflammation: Multiple sclerosis; Meningitis; Guillain-Barré syndrome
Correct Answer is C
Explanation
This is an incorrect answer. Papilledema is a condition that causes swelling of the optic disc, which can affect peripheral vision and cause headaches. Papilledema can occur in some clients who have increased intracranial pressure (ICP) due to various causes, such as brain tumors, meningitis, or hydrocephalus, but it is not a common finding in MS.
Correct Answer is ["A","B","C","E"]
Explanation
This is a correct answer. Positive Brudzinski sign is another common symptom of meningitis, which is flexion of the hips and knees when flexing the neck forward. Positive Brudzinski sign occurs due to the irritation of the spinal nerve roots by the inflamed meninges.
This is an incorrect answer. The nurse should not tell the client that they have GBS because they have been exposed to a virus that infects their nerve cells. This is not the cause of GBS, but rather encephalitis, which is an acute inflammatory condition of the brain that can be caused by various vi
This is a correct answer. Dimming the lights and reducing noise in the room is an effective intervention to relieve the client's symptoms of headache, nausea, and vomiting due to meningitis. Dimming the lights and reducing noise can decrease sensory stimulation and irritation of the optic nerve or c
Search Here
Related Topics
More on Nursing
- Pathophysiology of the Musculoskeletal System
- Pathophysiology of the Reproductive System
- Pathophysiology of the integumentary system
- Pathophysiology of the Hematologic System
- Pathophysiology of the respiratory system
- Pathophysiology of the renal system
- Pathophysiology of the Gastrointestinal System
- Basic Concepts of Pathophysiology
Free Nursing Study Materials
Access to all study guides and practice questions for nursing for free.
- Free Nursing Study Trials
- Free Nursing Video tutorials
- Free Nursing Practice Tests
- Free Exam and Study Modes
- Free Nursing Revision Quizlets
