The client asks the nurse about storing insulin. Which response by the nurse is correct?
Vials of insulin should be refrigerated.
Insulin will last longer if kept in the freezer.
Opened vials of insulin must be discarded.
Insulin pens never have to be refrigerated.
The Correct Answer is A
Choice A rationale:
Insulin is a protein-based hormone that is sensitive to heat and light. Exposure to high temperatures or direct sunlight can cause insulin to break down and become less effective.
Refrigeration helps to maintain the stability and potency of insulin. It is generally recommended to store unopened insulin vials in the refrigerator at a temperature between 36°F and 46°F (2°C and 8°C).
This temperature range helps to slow down the degradation process and ensure that the insulin remains effective until its expiration date.
Choice B rationale:
Insulin should never be frozen. Freezing can cause the insulin to crystallize and become unusable. Once insulin has been frozen, it cannot be thawed and used again.
Choice C rationale:
Opened vials of insulin do not need to be discarded immediately. They can be stored in the refrigerator for up to 28 days, depending on the type of insulin.
However, it is important to note the date that the vial was opened and to discard it after the recommended storage period.
Choice D rationale:
Insulin pens should be stored according to the manufacturer’s instructions. Some insulin pens can be stored at room temperature for a certain period of time, while others must be refrigerated.
It is important to read the instructions that come with the insulin pen to ensure that it is stored properly.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A rationale:
Stevens-Johnson syndrome (SJS) is a rare, serious skin condition that is typically caused by an allergic reaction to medication. While amiodarone has been associated with a few cases of SJS, it is not considered a common long-term side effect.
Choice B rationale:
Ventricular tachycardia (VT) is a type of fast heart rhythm that originates in the ventricles of the heart. Amiodarone is actually used to treat VT, so it would be counterintuitive to list it as a long-term side effect.
Choice C rationale:
Pulmonary fibrosis is a condition characterized by scarring of the lung tissue. While amiodarone can cause pulmonary toxicity, which includes pulmonary fibrosis, this is a relatively rare side effect. Moreover, it's usually associated with high doses or
long-term use of the medication.
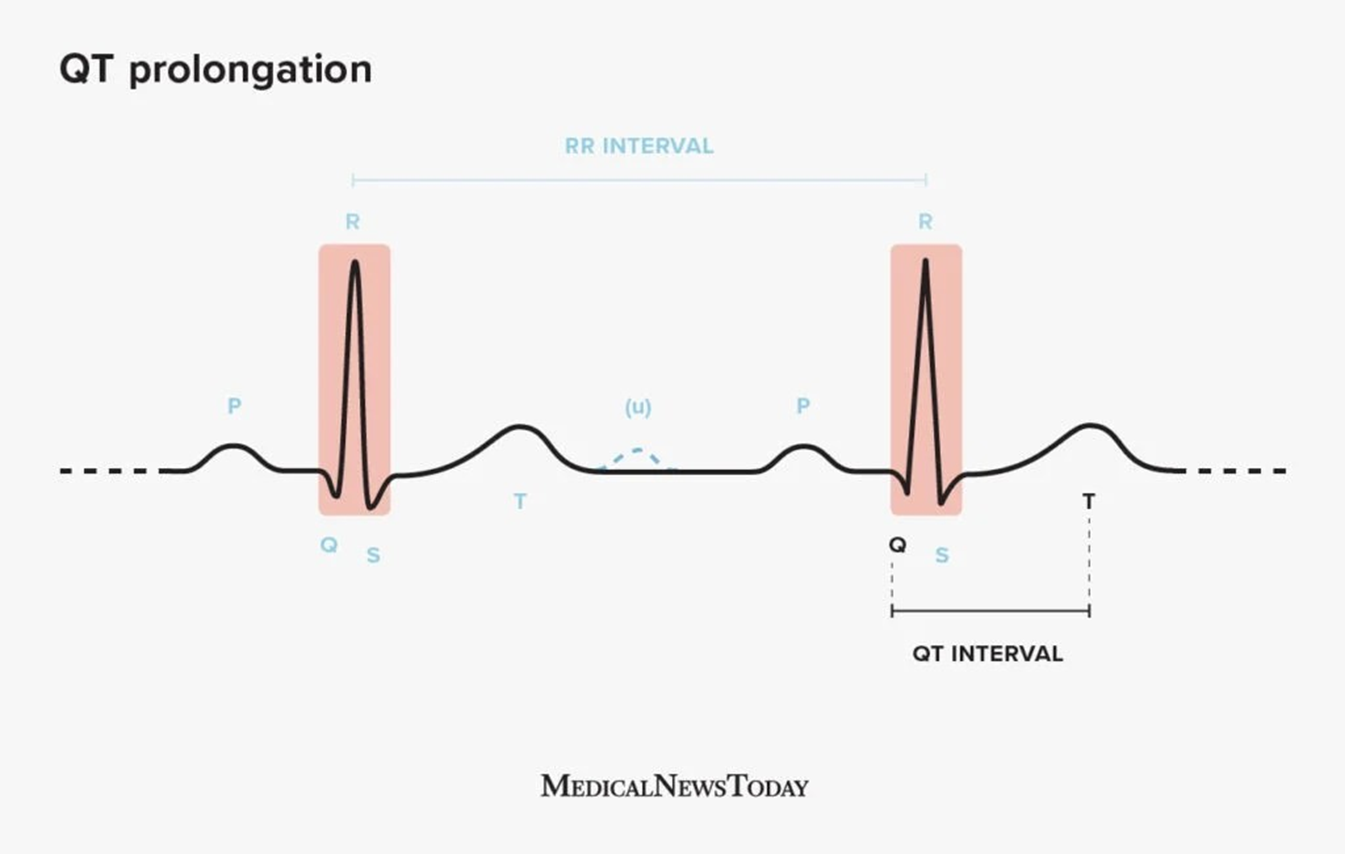
Choice D rationale:
QT prolongation is a condition in which the heart's electrical activity takes longer than normal to recharge between beats. This can lead to a potentially fatal arrhythmia called torsades de pointes. Amiodarone is known to prolong the QT interval, and this is considered one of its most significant long-term side effects. It's important to monitor patients on amiodarone for QT prolongation and to adjust the dose or discontinue the medication if necessary.
Correct Answer is B
Explanation
Choice A rationale:
COPD (Chronic Obstructive Pulmonary Disease) is a chronic lung disease that causes airflow obstruction. While labetalol can cause some bronchoconstriction, it is generally considered safe for use in patients with COPD. However, it's essential to monitor respiratory status closely, especially in those with severe COPD.
Choice B rationale:
Narrow-angle glaucoma is an eye condition characterized by increased intraocular pressure (IOP) due to impaired drainage of aqueous humor. Labetalol can exacerbate this condition by further increasing IOP through its beta-blocking effects. This can lead to acute angle-closure glaucoma, a medical emergency that can result in permanent vision loss.
Specific mechanisms by which labetalol can increase IOP:
Reduced aqueous humor production: Beta-blockers like labetalol can decrease the production of aqueous humor, the fluid that maintains eye pressure. While this might seem beneficial, a significant reduction can lead to anterior chamber shallowing, which can mechanically block the drainage angle and trigger angle closure.
Impaired uveoscleral outflow: Beta-blockers can also impair the uveoscleral outflow pathway, an alternative route for aqueous humor drainage that becomes more important in glaucoma patients. This can further contribute to IOP elevation.
Vasoconstriction of ciliary blood vessels: Labetalol's alpha-blocking effects can cause vasoconstriction of the ciliary blood vessels, which supply blood to the ciliary body responsible for aqueous humor production. This can reduce blood flow and indirectly hinder aqueous humor drainage.
Pupillary dilation: Beta-blockers can cause pupillary dilation, which can mechanically narrow the anterior chamber angle and obstruct aqueous humor outflow.
Therefore, labetalol is generally contraindicated in patients with known narrow-angle glaucoma.
Choice C rationale:
Hypertension (high blood pressure) is one of the primary indications for labetalol. It is an effective antihypertensive medication that works by blocking beta receptors, leading to decreased heart rate, contractility, and blood pressure.
Choice D rationale:
Tachycardia (fast heart rate) can also be treated with labetalol due to its beta-blocking effects. It helps to slow down the heart rate and restore a normal rhythm.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
