Which statement is true concerning osteogenesis imperfecta (OI)?
OI is easily treated
With a later onset, the disease usually runs a more difficult course
Braces and PT exercises are of no therapeutic value
OI is an inherited disorder
The Correct Answer is D
Choice A: OI is Easily Treated
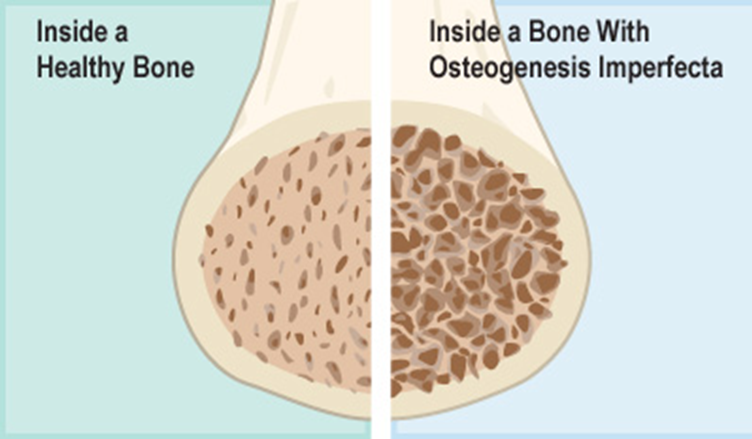
Osteogenesis imperfecta (OI) is not easily treated. It is a genetic disorder characterized by fragile bones that break easily. While there are treatments available to manage symptoms and improve quality of life, there is no cure for OI1. Treatments include medications to strengthen bones, physical therapy, and surgical procedures.
Choice B: With a Later Onset, the Disease Usually Runs a More Difficult Course
The severity of osteogenesis imperfecta can vary widely, but it is not necessarily true that a later onset leads to a more difficult course. The course of the disease depends on the type of OI and the specific genetic mutation involved. Some types of OI are more severe and present earlier in life, while others are milder and may not be diagnosed until later.
Choice C: Braces and PT Exercises are of No Therapeutic Value
This statement is incorrect. Braces and physical therapy (PT) exercises are valuable in managing osteogenesis imperfecta. Physical therapy helps in building muscle strength, improving joint movement, and preventing fractures. Braces can provide support for weak muscles, decrease pain, and keep joints properly aligned.
Choice D: OI is an Inherited Disorder
This statement is true. Osteogenesis imperfecta is a genetic disorder that is usually inherited in an autosomal dominant pattern. This means that a person only needs one copy of the defective gene from one parent to inherit the disorder. In some cases, OI can also occur due to a spontaneous mutation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A reason:
Bacteriuria, or the presence of bacteria in the urine, is not a primary clinical manifestation of acute renal failure. While facial edema can occur due to fluid retention, bacteriuria is more commonly associated with urinary tract infections. Acute renal failure primarily affects the kidneys’ ability to filter waste and regulate fluid and electrolytes, leading to symptoms such as oliguria and hypertension.
Choice B reason:
Hematuria, or blood in the urine, can be a symptom of various kidney conditions, but it is not a primary manifestation of acute renal failure1. Pallor, or paleness, can occur due to anemia, which may be a secondary complication of chronic kidney disease rather than acute renal failure. The primary symptoms of acute renal failure are related to the sudden decline in kidney function, such as oliguria and hypertension.
Choice C reason:
Proteinuria, or the presence of excess protein in the urine, is more commonly associated with chronic kidney disease or nephrotic syndrome rather than acute renal failure. Muscle cramps can occur due to electrolyte imbalances, but they are not primary manifestations of acute renal failure. The primary symptoms of acute renal failure include oliguria and hypertension.
Choice D reason:
Oliguria, or reduced urine output, and hypertension, or high blood pressure, are primary clinical manifestations of acute renal failure. Acute renal failure results in a sudden decline in kidney function, leading to the retention of waste products and fluids, which can cause oliguria and hypertension. These symptoms are key indicators of acute renal failure and require prompt medical attention.
Correct Answer is C
Explanation
Choice A reason:
A diet consisting of low-fat, low-carbohydrate foods is not specifically recommended for managing severe edema associated with acute glomerulonephritis. While a balanced diet is important, the primary dietary focus should be on reducing sodium intake to prevent fluid retention and manage edema. Therefore, this choice is not the most appropriate recommendation.
Choice B reason:
Decreasing the number of calories in the child’s diet is not a primary recommendation for managing severe edema associated with acute glomerulonephritis. The focus should be on reducing sodium intake rather than calorie restriction. Adequate nutrition is essential for the child’s overall health and recovery1. Therefore, this choice is not the most appropriate recommendation.
Choice C reason:
Avoiding adding salt to the child’s food is a key recommendation for managing severe edema associated with acute glomerulonephritis. Sodium can lead to water retention, which can worsen edema and increase blood pressure. A low-sodium diet helps to reduce fluid retention and manage the symptoms of glomerulonephritis. This is the most appropriate dietary recommendation for managing severe edema in this condition.
Choice D reason:
Increasing the amount of protein in the child’s diet is not recommended for managing severe edema associated with acute glomerulonephritis1. In fact, protein intake may need to be monitored and possibly restricted to prevent the buildup of waste products in the blood1. The primary dietary focus should be on reducing sodium intake to manage edema. Therefore, this choice is not the most appropriate recommendation.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
