A nurse is collecting data from a client who is 12 hours postpartum following a spontaneous vaginal delivery.
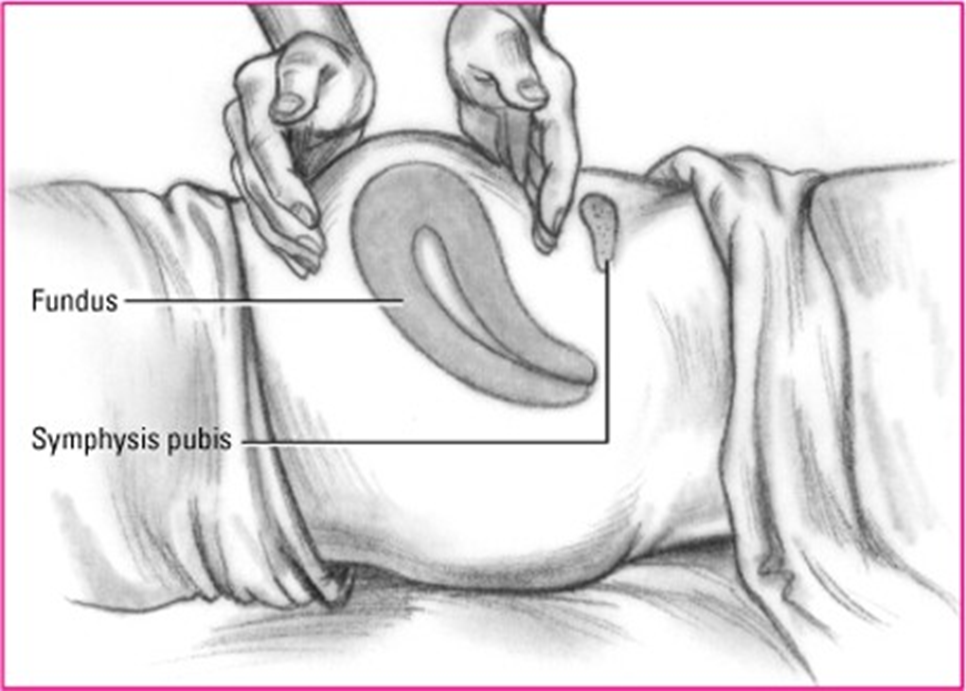
The nurse should expect to find the uterine fundus at which of the following positions on the client’s abdomen?
Three fingerbreadths above the umbilicus
At the level of the umbilicus
One fingerbreadth above the symphysis pubis
One fingerbreadth below the umbilicus
The Correct Answer is B
Choice A rationale:
Three fingerbreadths above the umbilicus is too high for the uterine fundus to be at 12 hours postpartum. Immediately after delivery, the fundus is typically at the level of the umbilicus. It then descends approximately one fingerbreadth per day.
If the fundus is found to be three fingerbreadths above the umbilicus at 12 hours postpartum, it could be a sign of uterine atony, which is a serious condition that can lead to postpartum hemorrhage.
Choice C rationale:
One fingerbreadth above the symphysis pubis is too low for the uterine fundus to be at 12 hours postpartum. This would be more consistent with a woman who is several days postpartum.
Choice D rationale:
One fingerbreadth below the umbilicus is also too low for the uterine fundus to be at 12 hours postpartum. This would be more consistent with a woman who is 1-2 days postpartum.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A rationale:
Gestational hypertension is a condition characterized by elevated blood pressure during pregnancy. While it can increase the
risk of certain complications, it is not directly associated with an increased risk of postpartum hemorrhage. This is because
gestational hypertension primarily affects the vascular system, not the uterine muscle function, which is responsible for
controlling postpartum bleeding.
Choice B rationale:
A small for gestational age newborn (SGA) is a baby who is smaller than expected for their gestational age. While SGA can be
associated with some pregnancy complications, it is not a direct risk factor for postpartum hemorrhage. The size of the baby
does not have a significant impact on the ability of the uterus to contract and prevent excessive bleeding after delivery.
Choice C rationale:
Precipitous birth is defined as a labor that progresses very rapidly, with delivery occurring within three hours or less of the
onset of regular contractions. This rapid progression of labor can lead to postpartum hemorrhage for several reasons:
Uterine atony: The uterus may not have enough time to contract effectively after a rapid delivery, leading to increased
bleeding.
Lacerations and trauma: The rapid passage of the baby through the birth canal can increase the risk of tearing of the cervix,
vagina, or perineum, which can contribute to blood loss.
Retained placenta: The placenta may not separate from the uterine wall as easily after a precipitous birth, increasing the risk
of hemorrhage.
Choice D rationale:
A two-vessel umbilical cord is a variation in which the umbilical cord contains only two blood vessels (one vein and one
artery) instead of the usual three (one vein and two arteries). While this can be associated with certain fetal anomalies, it is not
a direct risk factor for postpartum hemorrhage. The number of blood vessels in the umbilical cord does not significantly
impact the ability of the uterus to contract and prevent bleeding after delivery.
Correct Answer is C
Explanation
Choice A rationale:
Swelling in both breasts is a common finding in breastfeeding women, especially in the early postpartum period. It is often due
to engorgement, which is caused by an oversupply of milk and/or infrequent milk removal.
While engorgement can sometimes lead to mastitis, it is not a definitive sign of the condition.
Other causes of bilateral breast swelling, such as milk stasis or plugged ducts, should also be considered.
Choice B rationale:
Cracked and bleeding nipples can be a symptom of mastitis, but they are not always present.
They can also be caused by other factors, such as improper latch, thrush, or dry skin.
It is important to assess for other signs and symptoms of mastitis, such as fever, chills, and breast tenderness, to make a
definitive diagnosis.
Choice C rationale:
A red and painful area in one breast is a classic sign of mastitis.
This is typically caused by inflammation of the breast tissue, often due to a bacterial infection.
The redness and pain are usually localized to the affected area, and may be accompanied by warmth, swelling, and firmness.
Choice D rationale:
An increase in breast milk production is not a sign of mastitis.
In fact, it is often a sign that breastfeeding is going well.
However, if the milk is not being removed effectively, it can lead to engorgement and blocked ducts, which can increase the
risk of mastitis.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
