A nurse is caring for a client who develops an airway obstruction from a foreign body but remains conscious. Which of the following actions should the nurse take first?
Perform a blind finger sweep.
Turn the client to the side.
Insert an oral airway.
Administer the abdominal thrust maneuver.
The Correct Answer is D
Choice A reason: Perform a Blind Finger Sweep
Performing a blind finger sweep is not recommended because it can push the foreign object further into the airway, making the obstruction worse. This method is only advised if the object is clearly visible and can be safely removed without causing further harm.
Choice B reason: Turn the Client to the Side
Turning the client to the side can be helpful in certain situations, such as when the client is unconscious or at risk of vomiting. However, in the case of a conscious client with a foreign body airway obstruction, this action does not directly address the obstruction and is not the first priority.
Choice C reason: Insert an Oral Airway
Inserting an oral airway is typically used to maintain an open airway in an unconscious patient who cannot maintain their own airway. For a conscious client with a foreign body obstruction, this action is not appropriate and could cause further complications.
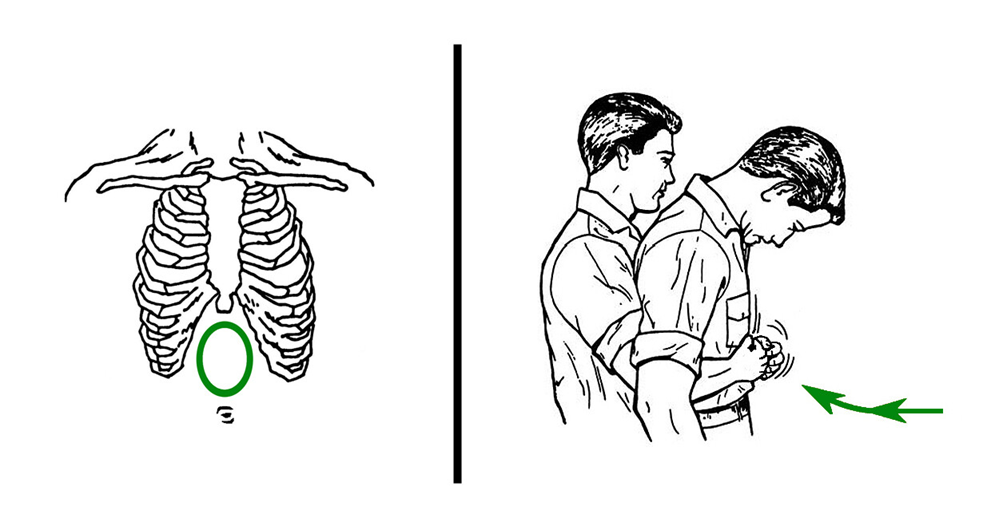
Choice D reason: Administer the Abdominal Thrust Maneuver
Administering the abdominal thrust maneuver (also known as the Heimlich maneuver) is the recommended first action for a conscious client with a foreign body airway obstruction. This technique involves standing behind the client, placing a fist just above their navel, and delivering quick, upward thrusts to expel the foreign object. This method is effective in creating an artificial cough that can dislodge the obstruction.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["D","E"]
Explanation
Choice A reason:
Don sterile gloves: While it is important to maintain cleanliness, sterile gloves are not necessary for administering a suppository. Clean, non-sterile gloves are sufficient to prevent infection and ensure hygiene.
Choice B reason:
Position the client supine with knees bent: The correct position for administering a suppository is the left lateral (Sims) position, not supine with knees bent. The left lateral position allows for easier access to the rectum and helps the suppository stay in place.
Choice C reason:
Use a rectal applicator for insertion: Suppositories are typically inserted using a gloved finger, not a rectal applicator. The gloved finger allows for better control and ensures the suppository is placed correctly.
Choice D reason:
Insert the suppository just beyond the internal sphincter: This is correct. The suppository should be inserted past the internal sphincter to ensure it stays in place and can dissolve properly. This placement helps the medication to be absorbed effectively.
Choice E reason:
Lubricate the index finger: Lubricating the index finger is essential to make the insertion process smoother and more comfortable for the client. It helps prevent trauma to the rectal mucosa and ensures the suppository is inserted easily.
Correct Answer is B
Explanation
Choice A reason: A Client Who Has a Small Circular Partial-Thickness Burn of the Left Calf
A small circular partial-thickness burn of the left calf is considered a minor injury in the context of a mass casualty event. This type of injury does not pose an immediate threat to life and can be managed after more critical cases are addressed. In mass casualty triage, patients with minor injuries are often categorized as “green” or “minimal” and are treated last.
Choice B reason: A Client Who Has Severe Respiratory Stridor and a Deviated Trachea
A client with severe respiratory stridor and a deviated trachea should be assessed first. These symptoms indicate a potential airway obstruction, which is a life-threatening condition requiring immediate intervention. In mass casualty triage, patients with compromised airways are given the highest priority and are categorized as “red” or “immediate” because their condition is critical and requires urgent medical attention.
Choice C reason: A Client Who Has a Splinted Open Fracture of the Left Medial Malleolus
A splinted open fracture of the left medial malleolus is a serious injury but not immediately life-threatening if properly splinted. This client would be categorized as “yellow” or “delayed” in mass casualty triage, meaning they require medical attention but can wait until more critical patients are stabilized.
Choice D reason: A Client Who Has a Massive Head Injury and Is Experiencing Seizures
A client with a massive head injury and experiencing seizures is in a critical condition. However, in the context of mass casualty triage, the immediate priority is to secure the airway, breathing, and circulation. While this client is in dire need of medical attention, the presence of severe respiratory stridor and a deviated trachea in another client takes precedence due to the immediate threat to life.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
