A nurse discovers that a client has been administered a higher dose of oxybutynin than the prescription indicates. The nurse should assess the client for which of the following adverse effects?
Increased salivation
Hyperthermia Urinary incontinence
Urinary incontinence
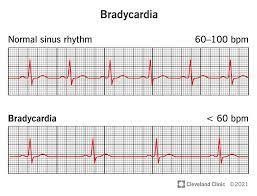
Bradycardia
The Correct Answer is D
Oxybutynin is an anticholinergic medication commonly used to treat urinary incontinence. One of the adverse effects of anticholinergic medications is the potential for bradycardia, which refers to a slower than normal heart rate. Anticholinergic medications can inhibit the effects of acetylcholine, a neurotransmitter responsible for regulating various bodily functions, including heart rate. Therefore, it is important to assess the client for signs of bradycardia after an unintended higher dose of oxybutynin.
Increased salivation (A) is not an expected adverse effect of oxybutynin. In fact, anticholinergic medications like oxybutynin often have the opposite effect, causing dry mouth and reduced salivation.
Hyperthermia (B) is not a typical adverse effect of oxybutynin. It is more commonly associated with other conditions or medications.
Urinary incontinence (C) is the condition that oxybutynin is intended to treat. It is not an adverse effect but rather the therapeutic effect of the medication.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
When providing teaching to a client with chronic rheumatoid arthritis who is starting a new prescription for hydroxychloroquine, the nurse should instruct the client to obtain routine eye examinations. Hydroxychloroquine is an antimalarial and immunosuppressive medication commonly used to treat rheumatoid arthritis and other autoimmune conditions.
One of the potential side effects of hydroxychloroquine is ocular toxicity, particularly affecting the retina. Retinal toxicity can lead to vision changes or, in severe cases, irreversible damage to the eyes. Therefore, regular eye examinations are necessary to monitor for any signs of retinal toxicity and detect any visual changes early to prevent further complications.
The American Academy of Ophthalmology recommends that patients taking hydroxychloroquine undergo a baseline eye examination before starting the medication and annual eye examinations thereafter, especially after five years of continuous use.
Let's go through the other options:
B. Chest x-ray: A chest x-ray is not routinely required for monitoring clients taking hydroxychloroquine for rheumatoid arthritis. Hydroxychloroquine is not known to cause significant respiratory or pulmonary side effects.
C. Pancreatic enzyme levels: Monitoring pancreatic enzyme levels is not specifically related to hydroxychloroquine therapy. Pancreatic enzyme level testing is typically used to assess the function of the pancreas in conditions like pancreatitis or pancreatic insufficiency.
D. Urinalysis screening: While regular monitoring of kidney function is important for clients on long-term medication therapy, routine urinalysis screening is not specifically related to hydroxychloroquine use in clients with rheumatoid arthritis. Regular eye examinations are of higher priority due to the potential ocular toxicity associated with this medication.
Correct Answer is B
Explanation
A nurse who is caring for a preschooler should question a prescription for tetracycline. Tetracycline is contraindicated in children under 8 years of age due to its potential to cause permanent discoloration and damage to developing teeth and bones. This adverse effect is known as tooth staining or dental hypoplasia.
Let's go through the other options:
A. Azithromycin: Azithromycin is an appropriate antibiotic for use in preschool-age children and is commonly prescribed for various bacterial infections. It does not pose the same risk of tooth staining as tetracycline, making it a safe option for this age group.
C. Cefuroxime: Cefuroxime is another antibiotic that is safe for use in preschoolers. It belongs to the cephalosporin class of antibiotics and is commonly prescribed for respiratory tract infections, skin infections, and other bacterial infections.
D. Gentamicin: While gentamicin is an effective antibiotic, its use in preschool-age children should be carefully monitored. Gentamicin can have potential ototoxic and nephrotoxic effects (damage to the inner ear and kidneys, respectively). However, its use is not strictly contraindicated in this age group, and it can be prescribed when necessary with appropriate monitoring.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
