A client with multiple sclerosis has urinary retention related to sensorimotor deficits. Which action should the nurse include in the client's plan of care?
Remind the client to practice pelvic floor (Kegel) exercises regularly.
Provide a bedside commode for immediate use in the client's room
Explain the need to limit intake of oral fluids to reduce client discomfort.
Teach the client techniques for performing intermittent catheterization.
The Correct Answer is D
A. Remind the client to practice pelvic floor (Kegel) exercises regularly.
Pelvic floor exercises, such as Kegel exercises, are typically recommended for conditions involving weakened pelvic floor muscles. However, in the context of urinary retention related to sensorimotor deficits in multiple sclerosis, the issue is more neurological in nature. Therefore, pelvic floor exercises may not address the underlying problem effectively.
B. Provide a bedside commode for immediate use in the client's room.
While a bedside commode may be beneficial for individuals with mobility issues, it doesn't directly address the problem of urinary retention. It focuses on providing a convenient means for the client to void when needed, but it doesn't address the inability to empty the bladder spontaneously.
C. Explain the need to limit intake of oral fluids to reduce client discomfort.
Limiting oral fluids is not an appropriate intervention for urinary retention. In fact, it could lead to dehydration, which is not a recommended approach. The focus should be on addressing the difficulty in voiding through appropriate techniques.
D. Teach the client techniques for performing intermittent catheterization.
This is the correct choice. Intermittent catheterization is a direct and effective method to manage urinary retention in clients with sensorimotor deficits. Teaching the client how to perform intermittent catheterization empowers them to maintain regular bladder emptying and prevent complications associated with urinary retention.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
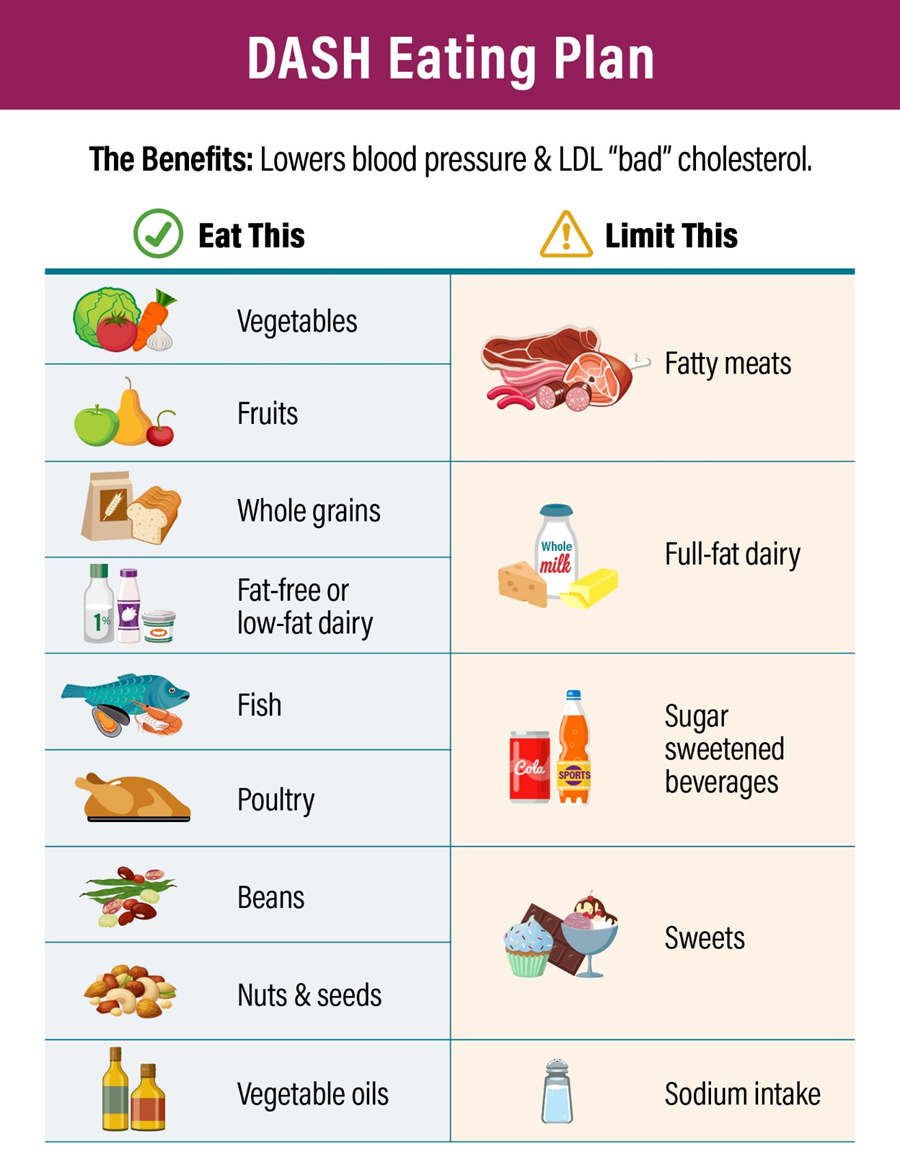
A. Carefully cleans and peels all fresh fruit and vegetables:
While cleaning and peeling fresh fruits and vegetables may contribute to food safety, it is not a specific indication of adherence to the DASH eating plan.
B. Uses only lactose-free dairy products:
The DASH eating plan encourages the consumption of low-fat or fat-free dairy products. Using lactose-free dairy products may be necessary for individuals with lactose intolerance, but it is not a specific behavior related to the DASH plan.
C. No longer includes grains in the daily diet:
The DASH eating plan includes whole grains as part of a balanced diet. Eliminating grains altogether is not consistent with the DASH plan, which encourages the consumption of whole grains.
D. Enjoys fat-free yogurt as an occasional snack food:
This is the correct answer. The DASH eating plan recommends the inclusion of low-fat or fat-free dairy products as part of a heart-healthy diet. Choosing fat-free yogurt as an occasional snack aligns with the principles of the DASH plan, which emphasizes low-fat dairy options.
Correct Answer is B
Explanation
A. Jugular vein distention:
Jugular vein distention is not typically associated with an increased risk of a stroke. It may be indicative of issues related to cardiac or fluid volume status.
B. Carotid bruit:
This is the correct answer. A carotid bruit, an abnormal sound caused by turbulent blood flow through the carotid artery, may indicate the presence of atherosclerosis and increased risk of stroke. It suggests a narrowing or blockage in the carotid artery, which can potentially lead to emboli and subsequent stroke.
C. Nuchal rigidity:
Nuchal rigidity, stiffness of the neck, is associated with conditions such as meningitis but is not a direct risk factor for a stroke.
D. Palpable cervical lymph node:
Palpable cervical lymph nodes may be indicative of infection or inflammation in the head and neck region but are not directly associated with an increased risk of a stroke.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
